The delivery of health services
around the world is changing rapidly, brought about by advances in surgical and
non-surgical treatments, the increasing aged population, funding pressures, and
the increased availability of self-help facilities and private healthcare
schemes. Less time is being spent in hospitals through advances in surgery
recovery times, pressures on beds, the availability of better home help
services, etc. This all requires a new model of the delivery of health
services provided in the home or in the community, ie not primary or secondary care
services provided in hospitals and doctors’ surgeries.
For the
purposes of this profile it is necessary to differentiate between what is
commonly called primary and secondary care, and home and community care. Primary
care refers to the work of healthcare professionals who act as a first point of
consultation for all patients within a healthcare system, and secondary care is
the healthcare services provided by medical specialists and other health
professionals who generally do not have first contact with patients. Home and community care refers to the many types of healthcare
interventions delivered outside of these primary and secondary facilities. It
includes the services of professionals in residential and community settings in
support of self care, home care, long-term care, assisted living, and treatment
for substance use disorders and other types of health and social care
services.
This profile
focuses on the latter category and describes how these future home and
community services can be delivered using new disruptive and interacting technologies
and using open standards developed by OASIS and other organizations.
Remote
Healthcare is just one facet of life that is made possible by the Internet of
Things (IoT) [Ref 11]. The IoT integrates physical objects into information
networks and allows those physical objects to become active participants in
business processes. This provides a basis for devices to monitor patients’
health, track and record exercise, sleep, and health information and to tell practitioners
whether treatment is being applied, and if so, how it’s working.
1.1 References (non-normative)
[Ref 1] Diagrams of e-Devices and other self-care
facilities see http://www.eprforum.no
[Ref 2] e-Device apps developed in USA
see http://video.msnbc.msn.com/rock-center/50582822#50582822.
[Ref 3] Technical University of Munich (TUM) research see http://www.tum.de/en/about-tum/news/press-releases/short/article/30440/
[Ref 4]
Edinburgh University research see http://www.bbc.co.uk/news/uk-scotland-22695278
[Ref 5] Public Supervision & Quality Assurance (PSQA)
see http://www.eprforum.no/product.php/Supervision-and-Quality-in-Home-care-services/50/
[Ref 6] e-Folder standard see http://www.eprforum.no/product.php/Standard-EPR-and-e-Folder/3/
[Ref 7] e-Device standard see http://www.eprforum.no/description.php/EPR-eDevice/5/
[Ref 8] OASIS BCM-EPR SC see https://www.oasis-open.org/committees/tc_home.php?wg_abbrev=bcm-epr
[Ref 9] CAM templates see http://www.eprforum.no/product.php/CAM-Template-EditorProcessor/37
[Ref 10] European Interoperability Framework (EIF)
version 2.0 see http://ec.europa.eu/isa/documents/isa_annex_ii_eif_en.pdf
[Ref 11]
The Internet of Things see http://en.wikipedia.org/wiki/Internet_of_Things
[Ref 12] Functional Mapping in agnostic
programmable Service Oriented Systems see http://www.eprforum.no/publ_images/File/eDevice_IoT/Functional_Mapping_CEN_OASIS.pdf
2
The e-Health TGF Profile
The Profile contained in this Committee Note contains
detailed information and guidance on using the TGF and other OASIS standards to
support the work of the home and community healthcare community. A full
explanation of the TGF is given in the TGF v2.0 and whilst this Committee Note
makes no attempt to re-write that document, it does “translate” the most
relevant parts into the language more appropriate for that community. It also
identifies in particular which of the Core Patterns and Policy Products are relevant
and where necessary elaborates them more specifically to the healthcare domain.
The Transformational Government Framework is a
practical “how to” standard for the design and implementation of an effective programme
of technology-enabled change at national, state, county or local government level. It sets out a managed process of
ICT-enabled change in the public sector, which puts the needs of citizens and
businesses at the heart of that process and which achieves significant and
transformational impacts on the efficiency and effectiveness of government.
The Framework is applicable to a variety of domains of government activity and
although the TGF talks primarily about the delivery of citizen-centric services
it is equally applicable to other areas of public sector business including healthcare in the home and community. The fundamental principles being that
the structures, governance, funding, culture, and stakeholder engagement are
all organized in a holistic way for the benefit of patients and healthcare practitioners, which has to be the primary objective of any e-Health
programme.
The TGF
makes the point that all around the world, governments at national, state, and
local levels face huge pressure to do “more with less” and every government
faces the challenge of achieving their policy goals in a climate of increasing
public expenditure restrictions. This situation is equally true for those
responsible for operating e-Health programmes and there are clear opportunities
to realize economic benefits through full citizen, business and private sector
stakeholder engagement in the development of home and community healthcare
programmes.
Advances in technology, such as the Internet of Things, and
mobile infrastructures are providing the devices and means of delivering
necessary healthcare services to locations away from hospitals and surgeries,
eg to patients’ homes, care homes, holiday homes, etc. Through the use of
these various devices and also online self-help facilities [Ref 1] patients can service their own
needs but at the same time trigger emergency help when the need arises. The
new disruptive technologies available today are helping to create
new markets and value networks, and displacing earlier technologies. This
includes handling health condition monitoring in real time enabling actions to
be taken before emergency help and resources are needed.
However a plethora of isolated and “lock in” solutions and smart
phone and tablet Apps that dominate the market today can through the use of new
interoperable and reusable service templates integrate and share
information through techniques such as functional mapping. [Ref 12].
Use of these
technologies and devices does not take away the need for face-to-face
interaction but they do enable that time commitment can be kept to a minimum
and thus reduce the burdens on the already over-stretched healthcare
resources. It also enables the desire of many patients today, especially the
elderly, to be independent and remain in their own homes rather than being kept
in hospital or in care homes.
Examples of the advances being made
are as follows:
-
doctors in USA [Ref 2] have
developed a number of apps that can run on a smart phone providing remote,
wireless diagnosis and monitoring that can lead to better and cheaper
healthcare and provide lifestyle changes for the patient . They are also
developing a remote wireless monitor that can be worn on the wrist to reduce
the need for constant visits to a hospital or surgery.
-
researchers at
the Technical University of Munich (TUM) [Ref 3], in collaboration
with business partners, have designed an assistive system for helping senior
citizens live at home by embedding a tablet computer in the wall. As well as
providing a central location where users can access all of the information they
need, such as family and emergency phone numbers, it also contains biosensors
that can measure vital signs so the system can recommend exercise or
medication, or alert a physician or mobile nursing service if the health
problem is critical.
-
researchers at
Edinburgh University [Ref 4] found that the blood pressure of
people who used a self-monitoring system in a six-month trial dropped further
than those who did not. A portable machine which lets people measure their own
blood pressure and send results directly to doctors is said to have improved
patient health. The portable system allowed patients to send readings to
doctors and nurses, who then checked the figures and, if necessary, contacted
the patient to discuss their health and medication.
Whilst the
technology exists today as these examples demonstrate, there is a need to
ensure that all the various devices can work together and provide a single view
of the patient’s care needs. Aspects such as patient choice and privacy must
also be considered. That is where the use of standards comes in and it requires
hardware and software providers to use these standards to ensure there is the
necessary interoperability that enables the required flows of data between
patients and healthcare practitioners.
In addition to making the various devices work
together, huge benefits can be achieved with a single system of data entry - as
more and more people are being discharged from hospitals sooner, with more
focus on management in the community, having that vital information about what
has been happening in either sector provides a more effective
prompt service to the patient. Much time is wasted in hospital in
trying to find out what has been happening in the community before admission,
and vice-versa, so if this information is readily available, more productive
time can be spent ensuring the patient gets the required treatment. And it
promotes better multi-disciplinary working if all health professional notes are
shared, because each professional's work is affected by another’s. Linking
these various records is valuable to monitor those patients who are at risk of
self neglect or isolation in the community, subject to patient choice and
privacy constraints.
There are a number of aspects that
need to be addressed in order to implement the new service model for home and
community healthcare. These are described in the following sub-sections.
Dealing with
global Internet information exchanges on a large number of different world
based connected national infrastructures requires the need to split the global
governance of the physical infrastructures and the private and public
controlled services running on them. Cloud technology should not exclusively be
controlled by private business enterprises; they need to co-operate with public
cloud services and be subject to quality standards (for example, the Norwegian Public
Supervision & Quality Assurance (PSQA) [Ref 5] approach). Cloud services should
show a clear split between the data and the software solutions. The data
should be preserved for “ever” but the software needs to be substituted and
changed according to the technology development. Today several national
governments are wasting enormous amounts of money on infrastructures run on
private software vendor’s regimes. Adaptive and agile templating requires a
clear split between shared data and the different interacting software
applications.
Ineffective
and inefficient progress can be seen in many countries where taxpayers’ money
is being wasted building unneeded isolated public networks with tied up
services not available for the citizens or other application business areas
such as:
-
Healthcare
networks
-
Smart Grid
networks
-
Police networks
-
Military networks
-
Emergency
networks
-
Broadcasting
networks
-
Tax system
networks
-
Road and Railroad
control networks
-
etc
However, it is important to realize that ‘one size
fits all’ is not usually a valid approach. For example, low-power free-to-use alternatives may be appropriate for
linking e-Devices where there are small amounts of data to transfer, where
battery life is an issue, and where network charges would make the application
uneconomic.
New thinking is required to differentiate between
the following 5 important related aspects:
1.
National communication
infrastructures - "Information Highways" the national
physical interacting packet switched IP-networks using basically Fibre and
4G-mobile networks.
- Shared
Data - shared persistent data in public registers.
- Abstract
Common and Open Service Models handling Information Exchange - downward semantic compatibility interacting on
the shared data.
- Traditional
Software programmes/platforms
- the software should be adapted
and substituted continuously according to new applications, legislations,
technology and methodologies. All information exchange should be done
through common certificated Service Models.
- Executing
legislated public services and buying care equipment - undertaken by both private and public
enterprises.
Today’s
typical mix of these 5 areas into silo and monopolistic systems of locked
vendor regimes do prevent the needed interaction reforms in public sector to
succeed, especially
regarding the often legislated public services needing a common national
interaction area indicated by 1, 2 and 3 above. This has to do with society’s
backbone responsibility of administrations tasks, not driven by profit goals,
but operating securely and enabling fair competition in areas 4 and 5 above for
business related software and attached services. Even if areas 1-3 are the
public sector’s responsibility, companies should be able to compete on common
terms to handle them, but these companies should be prevented from delivering
software programmes/platforms or services to avoid a monopolistic or
oligopolistic market situation.
The physical
implementation of this new service model will be by using the Internet to
enable standardized flows of data between patients and the executers of healthcare
services. Most of this data comes directly from the patient’s own monitoring
e-devices but also via self-help facilities. Through a neutral and public defined “Super Structure” it is
possible to demonstrate how to solve much of the rising healthcare interaction
problems related to the holistic approach of needed common information exchange
modelling. The interaction via the
Internet enables new ways of self diagnosis, self service and use of expertise
through new ways of frontline service management as covered in the TGF.
One
way of implementing this new agile meta-engineering is through the use of the Norwegian
EPR Public Supervision
and Quality Assurance programme ( PSQA ) [Ref 5] which is developing a common electronic
framework for the healthcare supervision and quality assurance of citizen
services and for the business enterprises involved.
PSQA is intended to be used
in all relevant healthcare supervisions and by the enterprises that need to
comply with the supervision requirements. It is based on international quality
standards and uses electronic folders that integrate and interact with the
underlying legacy and expert systems in general handling the service
management.
An important aspect is the
interaction between the workflow service management for service executers
dealing with the e-Folders [Ref 6] and
the condition monitoring and deviation response system handled by e-Devices [Ref 7] in real-time, home automation and body sensing
condition monitoring. Typical application areas are:
- Integrated e-Device
Condition monitoring ( Body and Environment adapted User Scenarios)
- Interaction of e-Folder
Service work, Planning and Reporting (task description, reporting and
inspection)
- Service Tools access
using the OASIS CAM Templating editor (role control by digital signature using
the OASIS PKI standard )
4.3 The Use of e-Folders
The solution to delivering the service management
described above is to extract the computer support into electronic folders. The
folders have a standard design with standardized functionality and give the
user access to all needed information and help in the performance of the task.
Access is given through "single sign on" and approved digital
signatures for identification. Special applications and expert systems can be
integrated into the folders.
Important properties of the use of e-folders being
introduced in Norway are:
·
The folders are a
framework. The framework has several purposes, a common access point for all
relevant information, in order to integrate under laying systems, to be used as
next generation of “front office". The framework will function by use of
open standards for processing XML-based templates. The folders will also be
able to use a number of other standards.
·
Integration of
applications and data will be controlled by commands (on demand). Applications
can be components in special applications, expert systems, and help for users
e.g. access on command is the opposite of permanent access. Access on command
belongs to a technology called loosely-coupled applications.
·
The folders are customized
(adapted) for the actual need. This means that only correct and needed
information will be available through the folders.
·
The folders are
dynamic; they can be extended or reduced as needed. This is possible because of
the standardized structure that the folders have been designed around. The
structure is the base for automatic modeling of generic information.
The principles around customized folders
and access on command are important components in order to avoid unnecessary
dispersion of information. In addition to clear role structure this is
especially important in order to protect sensitive information and to protect
personal integrity.
4.4 The Use of e-Devices
Environmental
control and patient condition monitoring through interoperating electronic
equipment is crucial for self-centric healthcare management. Work is ongoing
within the OASIS BCM-EPR Sub-Committee [Ref 8] to produce a functional standard for e-Devices. The standard sets down the Methodology for Condition
Monitoring and the environmental
access control template management. It represents a standardized functional
mirrored model of electronic network devices (nodes) that are connected to
e-Folders content through Web services technology. It is derived from the
ANSI/CEA-721 work developed over the last 25 years by more than 400 companies,
organizations and individuals. The standard demonstrates how all the real open
BUS-technology standards can interact through a common top level real open XML
based functional modelling layer.
Many of the
standards required to support the delivery of the services described above have
been developed by OASIS.
The three described below provide the means of defining and developing the
specific model for the home and community service care.
The most relevant characteristics of the TGF approach that
support this new healthcare service model are:
- it takes a whole-of-government
view of the relationship between the public sector and the citizen. This
provides the correct working environment for the new service model to be
developed through the use of joined-up resources across agencies, the
sharing of data, the use of common rules and procedures, etc.
- it recognizes the need to
e-enable the whole frontline of public services: that is, including staff
and organizations involved in direct, personal delivery of services (such
as healthcare) as well as e-enabling transaction-based services.
Using the
TGF approach will ensure an effective programme of change can be developed to
deliver the services for the new home and community care model. It will ensure
that all the necessary stakeholders are involved, that resources are correctly
identified and managed, and that the envisaged benefits and outcomes are
achieved.
4.5.2
Business-Centric Methodology (BCM)
The
Business-Centric Methodology is a specification that provides business managers
with a set of clearly defined methods with which to acquire agile and
interoperable e-business information systems within communities of interests. It provides managers with a clear
understanding of what the business goals and appropriate steps are that need to
be applied for a specific project to succeed.
The BCM efforts
are on communication at three levels: (1) lexical, (2) semantic, and (3)
pragmatic interoperability for sets of Community of Interest (CoI), eg healthcare.
The BCM templates collect objectives and rationale for pragmatic
interoperability by recording and sharing design decisions along with artifact
data. The layered BCM products relate one or more artifacts together by
including rich metadata on each link for semantic interoperability. The BCM
combines together these components and calls for their management within an
information architecture founded on conceptual agreements (lexical).
The
complex interrelationships between business functions, the need for role-based
access control to them and the need for a common vocabulary and semantics all
require a standardized method for ensuring effective interoperability and
exchange of information. The Content Assembly Mechanism specification provides a generalized
assembly mechanism using templates of business transaction content and the
associated rules such as those produced by functional mapping [Ref 12].
Information exchanges are moving to technical formats using XML technology
worldwide. However XML by itself is only a mark-up language, it was never
intended to support exacting business interchange definitions, rules and
industry vocabularies. To provide that extra level of robust information
definition and exact control CAM has been developed to enable business users to
quickly and easily use templates to declaratively assert these missing business
rules and structural information requirements.
Working
examples [Ref 9] using the CAM editor have been developed to make the necessary
template models for 3 e-Device health units, a SmartGrid Light sensor, a
Thermostat and an Electrical meter, and more are being developed.
The Transformational Government Framework (TGF)
Standard is expressed as a series of Core Patterns. The rationale for using
the Pattern Language approach and the format of them is set out in the TGF v2.0
document and that should be read in conjunction with this Section.
Most if not all of the TGF Core Patterns are relevant
to the healthcare community. Some are very generic to all domains of
government activity and therefore require no further explanation in this Profile.
The full text of them is available in the TGF v2.0 document. However some are
considered essential for e-Health programmes and these are shown in full below suitably
tailored for that community but include references to the main TGF Core
Patterns.
Context
First among the [GP1] Guiding
Principles is the need for [B2] Program Leadership to develop a clear, compelling and shared
vision for the e-Health transformation program.
v v v
The Problem
It is not the intent of the Transformational Government
Framework to describe some perfect “end-state” for governments and healthcare
communities. All communities are different: the historical, cultural, political,
economic, social and demographic context within which each operates is
different, as is the legacy of business processes and technology implementation
from which it starts. So the Transformational Government Framework is not a
“one-size-fits-all” prescription for what a healthcare community should look
like in future.
Rather, each e-Health program needs to set its
own clear vision. This will require agreement and clarity amongst stakeholders
on:
·
the social, economic and/or environmental impacts that the program
seeks to achieve;
·
the challenges that an e-Health program needs to overcome
in order to deliver these impacts and the vision should address – such as, for
example:
−
Healthcare
budget pressures
−
Changing
patient needs
−
Patient
choice
−
Patient
privacy
−
Advances in surgical
and non-surgical treatments
−
Infrastructure
stress
−
Resource
scarcity
−
Skills and
market access
−
Growing
population
−
Aging
population
−
Mobile
population
−
Economic
inequality
−
Digital
divide
· how the future
will “feel” different for key stakeholders – so that the vision is articulated
not in technical terms, but also in human and emotional ones.
v v v
The Solution
Program Leadership must create a vision for
the e-Health program that:
a) is developed in an
iterative and collaborative manner (that is, inclusive of all stakeholder groups and informed by
patient and practitioners research and engagement, with social media and other
technologies used to enable wide public participation in the process);
b) embraces the
opportunities opened up by new technologies and delivery channels, open data
and effective collaboration;
c) does so in a way which
integrates these with the core socio-economic, political and environmental
vision for the future, rather than seeing them as somehow separate from the
healthcare management’s core strategic objectives;
d) can be measured.
v v v
Linkages
The vision should be informed by the TGF program’s [GP1] Guiding
Principles, and developed through intensive [B5]
Stakeholder Collaboration. It is
vital to ensure that the vision can be expressed in terms of measurable
outcomes and that clear “line of sight” is established between all activities
in the roadmap and delivery of these outcomes for the program vision. Guidance
on how to do this effectively is set out at TGF v2.0 Section 7 Benefit
Realization.
Context
A central task of the [B2] Program
Leadership and [B5] Stakeholder Collaboration is to enable the
machinery of government to deliver customer-centric services. The principles
set out in that Pattern apply equally to the leadership of the e-Health
programme and the delivery of care and services to patients. They need to
cooperate with all stakeholders in developing a new business model that
delivers that care and other services in practice, when and where they are
needed.
v v v
The Problem
The failure to create an appropriate
new operating model has arguably been the greatest weakness of most traditional
healthcare programs. The transition to e‑Health has involved overlaying
technology onto the existing operating model of the health care sector: an
operating model based around existing functionally-oriented departments,
agencies and practitioners. These behave like unconnected silos in which
policy-making, budgets, accountability, decision-making and service delivery
are all embedded within a vertically-integrated delivery chain based around delivery
functions rather than patient needs.
The experience of healthcare communities
around the world over the last two decades has been that silo-based delivery of
services simply does not provide an effective and efficient approach to
e-Health. Many attempts have been made to introduce greater cross-community
coordination, but largely these have been "bolted on" to the
underlying business model, and hence experience only limited success. Without
examination of, or fundamental change to, the underlying business model level,
the design and delivery of care and services remains fragmented and driven by the
structures of the community, rather than the needs of the patients.
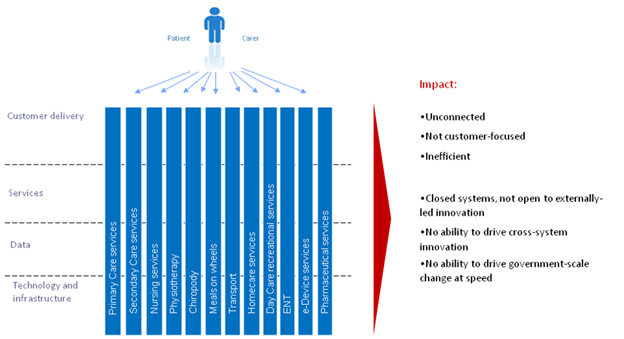
Figure
3 below illustrates the traditional operating model which is still typical of
most governments and healthcare communities:
·
the
individual patient usually has to engage separately with each silo: making
connections for themselves, rather than receiving seamless and connected
service that meets their needs;
·
data
and information has typically been locked within
these silos, limiting the potential for collaboration and innovation across the
community, and limiting the potential to drive change at speed.
Figure 3 – Traditional operating model: where healthcare
communities have come from
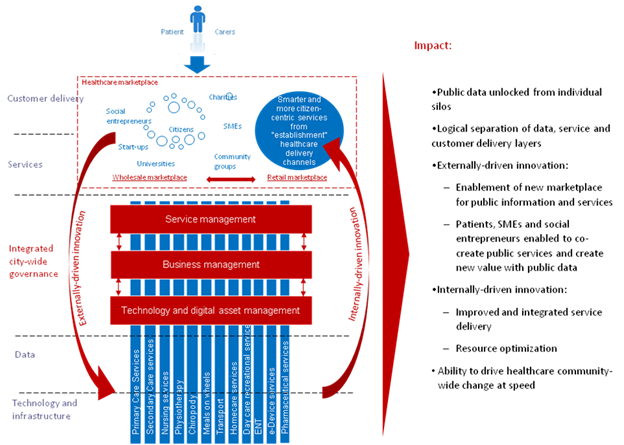
Healthcare transformation programs involve a shift in
emphasis, away from silo-based delivery and towards an integrated,
multi-channel, service delivery approach: an approach which enables a
whole-of-community view of the patient and an ability to deliver services to
patients where and when they need it most, including through one-stop services
and through private and voluntary sector intermediaries.
Key
features of this shift to a transformational operating model include:
a) investing
in smart data, i.e. ensuring that data on the performance and use of
the healthcare community’s physical, spatial and digital assets is available in
real time and on an open and interoperable basis, in order to enable real-time
integration and optimization of resources;
b) managing
public sector data as an asset in its own right, both within the
community and in collaboration with other significant data owners engaged in
the e-Health program;
c) enabling externally-driven, stakeholder-led innovation by patients, carers, communities and the private and voluntary
sectors, by opening up data and services for the common good:
· both at
a technical level, through development of open data platforms;
· and at
a business level, through steps to enable a thriving market in reuse of public
data together with release of data from commercial entities in a commercially
appropriate way;
d) enabling internally-driven, practitioner-led innovation to deliver more sustainable and patient-centric
services, by:
·
providing
patients with healthcare and services, which are accessible in one stop, over
multiple channels, that engage patients, carers, specialists and communities
directly in the creation of services, and that are built around patient needs
not the healthcare community’s organizational structures;
·
establishing
an integrated business and information architecture which enables a whole-of-health
service domain view of specific patient groups for e-Health services (e.g.
elderly people, drivers, parents, disabled people);
e) setting holistic and flexible budgets, with
a focus on value for money beyond standard departmental boundaries;
f) establishing community-wide governance and stakeholder management
processes to support and evaluate these changes.
Figure
4 summarizes these changes to the traditional way of operating which
transformational healthcare programs are seeking to implement.
Figure 4 – New integrated operating model: where healthcare
communities are moving to
v v v
The Solution
e-Health programs should therefore ensure that their [B1] Vision for Transformation includes the need to establish
a Transformational Operating Model to help build healthcare services around
patient needs, not just healthcare community’s organizational structure. This
will include:
- providing patients with healthcare and services
which are accessible via a common point or contact (generally a
specialist) and ideally offered over multiple channels, where appropriate;
- enabling those services also to be delivered by
private and voluntary sector intermediaries.
The Transformational Operating Model must go beyond
simple coordination between the existing silos and should include:
- An integrated
business and information architecture which enables a whole-of-patient
view, thus making possible both the integration of services and simple,
effective cross-organizational patient journeys;
- Incentives and business processes that encourage
the internal cultural change and cross-silo collaboration needed to drive
the integration and joining-up of services;
- A cross-community strategy for shared
development, management and re-use of common patient data sets,
applications, and applications interfaces (e.g. authentication, payments,
and notifications);
- Opening up public data for re-use and innovation
by the private and voluntary sectors, and directly by patients.
v v v
Linkages
Rather than attempting to restructure healthcare
communities to deliver such a Transformational Business Model, the [B4]
Franchise Marketplace SHOULD be considered as the recommended approach to
implement this model. Multi-channel delivery of services can be provided
through optimized [S6] Channel Transformation and public data can be
opened up to create new sorts of value through [S1] Stakeholder
Empowerment. Common patient data sets can be built as shared services with
customer data under customer control and managed using [T2] Technology
Development and Management. This pattern is facilitated by placing patient
and organizational data under their control as set out in [S3] Identity
and Privacy Management.
Context
Effective
stakeholder collaboration is critical. Establishing a process of sustainable
change requires a critical mass of actors inside and outside of the Home and
Community practitioners to be both engaged and supportive. Delivering a [B1]
Vision for Transformation cannot be done without meaningful stakeholder
collaboration.
The public, private, voluntary and
community healthcare sectors have considerable influence on patients’ attitudes
and behavior. These influences must be transformed into partnerships which
enable the market to deliver programme objectives. This requires a “map” of all
stakeholders as part of overall business management.
v v v
The Problem
It is not enough to map and understand stakeholder
relationships and concerns. Classic models of stakeholder engagement also need to be re-assessed.
Leaders from all parts of the health organization, as
well as other organizations involved in the program, need to be motivated for
the program to succeed and need to be engaged in clear and collaborative
governance mechanisms to manage any risks and issues. The development and
delivery of an effective e-Health program requires engagement with a very wide
range of stakeholders, not only across the whole of government but also, in
most cases, with one or more of the private, voluntary and community healthcare
sectors as well as with patients and other service customers. A significant
effort is needed to include all stakeholders in the governance of the e-Health
program at an appropriate and effective level.
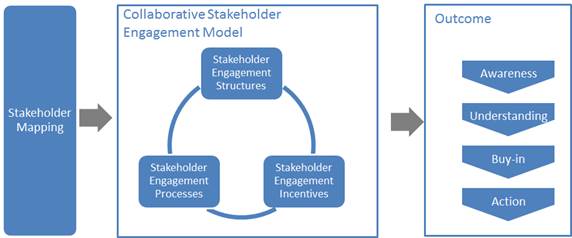
Key elements are set out below that a conformant
e-Health program will need to address in developing its Collaborative
Stakeholder Governance Model, if it is to engage successfully with stakeholders
and align them effectively behind shared objectives.
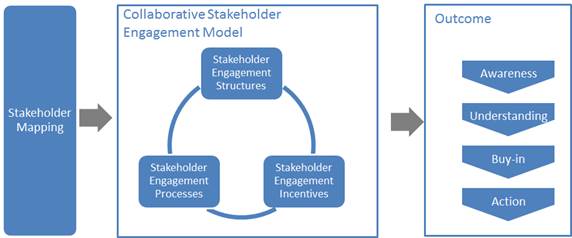
Figure 6: Overview of
Collaborative Stakeholder Governance
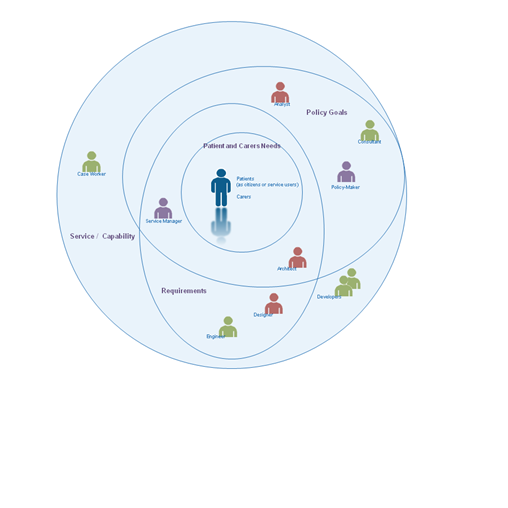
It is vital to describe and map the complete landscape
of relevant stakeholders. The
Transformational Government Framework puts the individual – whether acting on
their own behalf as a citizen or on behalf of another citizen or of a business–
at the centre:
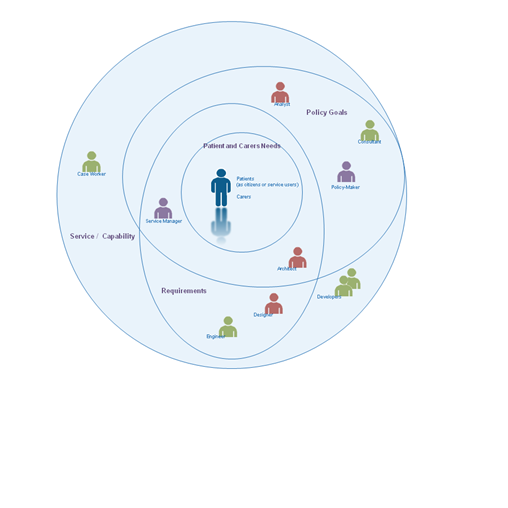
Figure 7: Landscape
of some key stakeholders
This view deliberately and completely
avoids the rather generic concept of ‘User’ that is dominant in traditional IT
stakeholder engagement models, preferring rather to identify the different
interests and concerns that are at stake (the mauve labels) and the key groups
of stakeholders (the different people icons) in the development of any service.
The figure is by no means complete nor the only
‘valid’ view. It seeks instead to illustrate that the process of transformation
requires reappraisal of the current set-up and assessment of what needs to
change.
By clearly separating out key stakeholder
groups and starting to understand and articulate their specific concerns as
stakeholders (any individual’s role may vary according to context:
in one situation, a person is a parent; in another, a policy-maker; or another,
a service provider), we can start to understand how stakeholders relate (in
different roles): to each other; to various administrations and services involved;
to policy drivers and constraints; and how these all come together in a
coherent ecosystem supported by a Transformational Government Framework. In
this view:
A service
(or ICT capability made available as a service) is understood as responding to
a set of requirements and policy goals (some of which overlap) – stakeholders
concerned at this level include, for example, case workers in a public
administration or developers who have worked with them in delivering a specific
service;
Requirements
encapsulate and formalize vaguely stated goals and needs of patients, carers
and businesses and take on board the policy goals of the political sponsor or
champion – stakeholders at this level include, for example, managers of public
service who can articulate the needs of their respective services, the
information and systems architects who capture those needs as formal
requirements that engineers can work with to develop services;
Policy
Goals capture the high-level concerns
and priorities of the political and health authorities and continually assess
how these goals reflect key patient and service delivery concerns –
stakeholders include policy makers and senior management as well as consultants
and analysts involved in helping identify technology and administrative trends
that can be used to leverage those goals; and finally;
Patient, carer and specialist needs that,
ultimately, can only be fully understood by the people concerned themselves –
nonetheless stakeholders at this level can also include patient or business
associations, consumer and other interest groups who engage with policy makers
to advance the interests of certain groups with distinct needs and are able to
articulate those needs in ways that can be used by analysts and consultants.
The various ellipses in the diagram above are
deliberately not concentric circles. This is to underline that the process of
establishing a service or capability is not a linear one going from needs,
goals and requirements. In reality stages are often inter-related.
The mapping of stakeholders and their principal
concerns at a generic level is used as a key input to the TGF [B9] Reference
Model and that needs to be validated within any e-Health program. It is
valuable as a tool for encouraging collaborative governance as it renders
explicit many of the relationships and concerns that are often left implicit
but nonetheless impact on an organization’s ability to reflect stakeholders’
concerns.
However, it is not enough simply to map
and understand stakeholder relationships and concerns. An effective e-Health
program will also address the three other dimensions of the model illustrated
above:
Stakeholder Engagement Structures: the organizational arrangements put in place to lead
the transformation program, e.g.:
-
central unit(s)
-
governance boards
-
health communities.
Stakeholder Engagement Processes: the processes and work flows through which the
e-Health Leadership and the different Stakeholders interact, e.g.:
-
reporting and
accountability processes
-
risk management processes
-
issue escalation
processes
-
consultation processes
-
collaborative product development
processes.
Stakeholder Incentives: the set of levers available to drive change through
these governance structures and processes. These will vary by jurisdiction, but
typical levers being deployed include:
-
central mandates
-
political leadership
-
administrative
championship
-
personal performance
incentives for healthcare professionals
-
alignment between public policy
objectives and the commercial objectives of private sector partners.
There is no one right model for doing this
successfully, but any conformant e-Health program needs to make sure that it
has used the framework above to define its own Collaborative Stakeholder
Engagement Model which explicitly articulates all of these elements: a
comprehensive stakeholder map, coupled with the structures, processes and
incentives needed to deliver full understanding and buy-in to the program, plus
effective stakeholder action in support of it.
Collaboration between e-Health Programs
The model clearly focuses attention within any
specific e-Health program. However (and increasingly) collaboration is required
also between governments and healthcare communities and, by implication,
between e-Health programs. In the figure below, we see that collaboration
between e-Health programs is favoured at the political, legal and
organizational levels and only later, if and when necessary, at the more
‘tightly-coupled’ semantic and technical levels.

Figure 8: Collaboration between eHealth
programs through different levels of Interoperability
This approach is also consistent with the SOA paradigm
for service development – not only are requirements defined and services
offered independently of any underlying technology or infrastructure but also
one e-Health program can be seen (and may need to be seen) as a ‘service
provider’ to another e-Health program’s ‘service request’. For example, a patient
wishing to use healthcare facilities in a second country may need to provide
authenticated information and credentials managed by the government or health
care community in the first country.
A further advantage of this approach is that it
becomes easier to identify and manage high level government requirements for
services: whether in the choice of ICT standards that may need to be used to
address a particular technology issue or determining the criteria for awarding
public procurement contracts, this approach allows a ‘loose-coupling’ at the
level of clearly defined high-level policy needs rather than the more
tightly-coupled and often brittle approach of specifying particular
technologies, software or systems.
v v v
The Solution
e-Health programs should establish, and give high
priority and adequate resources to, a formal managed
stakeholder engagement program. This should be led by a senior executive
and integrated into the roles of all involved in delivering the e-Health
program, and should cover:
·
Stakeholder
modelling: identifying and mapping the relationships
between all key stakeholders in the program (patients, healthcare professionals, suppliers,
delivery partners elsewhere in the public, private and voluntary sector,
politicians, the media, etc.); maintaining and updating the stakeholder model
on a regular basis;
·
A collaborative
stakeholder governance model: establishing
a clear set of structures, processes and incentives through which the [B2]
Program Leadership and the different stakeholders will interact, and covering:
‒ stakeholder
participation: ensuring
that all stakeholders have a clear understanding of the e-Health program and
how they will benefit from it, and
have effective and inclusive routes (including through use of digital media) to
engage with and participate in the program;
‒ cross-sectoral
partnership: engaging
effectively with stakeholders from the private, public and voluntary sectors to
deliver the program in a way that benefits all sectors;
‒ engagement with other e-Health programs to learn lessons and exchange experience.
v v v
Linkages
Stakeholder Collaboration should be established as a
formal workstream within the [B10]
Roadmap for Transformation, with measurable performance metrics built into the Benefits Realization framework. Stakeholder engagement underpins all other parts of
the e-Health program, because anyone in involved in the realization of the [B1] Vision for Transformation (or receiving benefits as a result) is considered a
stakeholder. However, intensive multi-stakeholder engagement is particularly
important for [B1] Vision for
Transformation, [B2] Program Leadership, [B7] Supplier Partnership, [S2]
Brand-led Service Delivery, [S1] Stakeholder
Empowerment and [S3] Identity and Privacy Management. The development of successful customer franchises
within the [B4] Franchise Marketplace will depend on the
effectiveness of collaborative governance – while at the same time helping
improve stakeholder collaboration significantly.
Context
In any e-Health programme it is vital that all
stakeholders have a common understanding of the key concepts involved and how
they interrelate, and have a common language to describe these in.
v v v
The
Problem
Leadership and communication both break down when
stakeholders understand and use terms and concepts in very different ways,
leading to ambiguity, misunderstanding and, potentially, loss of stakeholder
engagement.
In everyday life, we use terms –
‘citizen’, ‘need’, ‘service’ – as common, often implicitly accepted labels for concepts.
The concept is the abstract mental idea (which should be universal and language
independent) to which the term gives a material expression in a specific
language. Particularly in an international environment such as global
standardization initiatives, the distinction is important as it is common
concepts that we wish to work with, not common terms.
This distinction also helps avoid common modeling
pitfalls. Terms that may seem similar or the same across two or more languages
may actually refer to different concepts; or a single term in one language
could be understood to refer to more than one concept which another language
expresses with discrete terms: For example, the English term ‘service’
can refer to different concepts - an organizational unit (such as
‘Passport Service’ or ‘Emergency Services’) or something that is performed by
one for another (such as ‘a dry cleaning service’ or ‘authentication service’),
whereas discrete terms are used for the discrete concepts in German (‘Dienst’
or ‘Dienstleistung’ respectively for the two examples above). As the TGF is
intended for use anywhere in the world, it is important to ensure that
(ideally) global concepts can be transposed and translated and thus understood
in other languages: we therefore need to associate an explicit definition with
each concept as we do in a dictionary. The TGF uses a standard structure and
methodology to create its terminology and we recommend that such an approach should be
maintained in any extension of the terminology.
Concepts do not exist in isolation. In addition to
clear definitions and agreed terms, It is the broader understanding of the
relationships between concepts that give them fuller meaning and allow us to
model our world, our business activities, our stakeholders, etc. in a way that
increases the chance that our digital systems are an accurate reflection of our
work. Any conformant community should be able to use a common terminology
without ambiguity and be sure that these terms are used consistently throughout
all work.
v v v
The
Solution
Ensure that all stakeholders have a clear, consistent
and common understanding of the key concepts relating to healthcare in the home
and community; how these concepts relate to each other; how they can be
formally modeled; and how such models can be leveraged and integrated into new
and existing information architectures. It is particularly important that there
is a common understanding of the various terms associated with e-devices and
their usage. To this end:
Seek agreement among stakeholders to establish and
maintain an agreed and shared Common Terminology and Reference Model.
v v v
Linkages
Introduction to Terminology
A core terminology is proposed below and any e-Health
program should consider this as a basis for its own terminology and reference
model. It should be noted that this glossary is an extension of the main TGF
Core Terminology as set out in the Transformational Government Framework (TGF)
Version 2.0 and those terms should also be used wherever appropriate.
The TGF does not include a formal ontology but is
sufficiently clear in its concepts, definitions and relationships between
concepts that subsequent ontology development is possible if so desired.
Each entry below consists of a preferred
Term followed by the Definition (indented). Words in bold
within a definition refer to other terms defined within this core terminology.
Occasionally, a definition is followed by a note to clarify some element of the
definition or term.
e-Health Terminology
e-Device
any
piece of equipment that is used for environmental
control and patient condition monitoring and to and from which patient data is
transmitted electronically to healthcare practitioner(s)
e-Health
healthcare
practices supported by electronic processes and communication between
practitioners and patients using the Internet or other ICT networks
Functional Mapping
the description
of what needs to be done when transferring one value into another value with a
corresponding meaning
Healthcare
the diagnosis, treatment,
and prevention of disease, illness, injury, and other physical and
mental impairments in humans
Note: Healthcare is delivered by
practitioners in medicine, optometry, dentistry, nursing, pharmacy, allied health, and other care providers. It refers to the work done in
providing primary care, secondary care and home and community
care, as well as in public
health.
Home and community care
the many
types of healthcare interventions delivered outside of the primary and secondary
care facilities
Note: It includes the services of professionals in
residential and community settings in support of self care, home care, long-term
care, assisted living, and treatment for substance use disorders and other
types of health and social care services.
Internet of Things (IoT)
a
world where physical objects are seamlessly integrated into the information
network, and where the physical objects can become active participants in
business processes.
Note:
Services are available to
interact with these 'smart objects' over the Internet, query and change their
state and any information associated with them, taking into account security and
privacy issues.
Primary care
the work
of healthcare professionals who act as a first point of consultation for all
patients within a healthcare system
Secondary care
the
healthcare services provided by medical specialists and other health
professionals who generally do not have first contact with patients
5.5 Core
Pattern T2 - Technology Development and Management
Context
In
order for [T1]
Digital
Asset
Mapping and Management to be effective in
aligning healthcare technology and digital assets with the integrated, non-silo
based approach set out in [B3] Transformational Operating Model, it is
essential to have a top-level vision and architecture for future technology use
across the healthcare community.
v v v
The Problem
Technological change is more rapid than organizational
change and yet healthcare communities often find themselves locked-in to
particular technology solutions. Communities need to protect themselves against
the downside of technology evolution by developing a strategic approach to IT
that guarantees future agility as markets develop and healthcare priorities
change.
Transformational healthcare needs a strategic IT
platform to guarantee future agility as patient and practitioner priorities
change. Such a platform cannot afford to be locked-in to specific technologies
or solutions that prevent or limit such agility.
·
a commitment to the
paradigm and principles of Service Oriented Architecture (SOA) and SOA-based infrastructure, as defined
in the OASIS ‘Reference Model for Service-Oriented Architecture [SOA-RM]. Service-Oriented Architecture must be
understood in its broadest sense – as a paradigm for organising and using
capabilities distributed and managed across different ownership domains. In
this sense, SOA is technology and platform agnostic and thus provides an
appropriate foundation for the technology management framework.
·
modular
design,
including the realization of discrete care and services that can perform work
on behalf of other parties, underpinned by clear service descriptions and
contracts for any capability that is offered for reuse by another party;
·
clear
ownership and governance for all blueprint elements;
·
shared services: managing key ICT building blocks as
community-wide resources available as re-usable, shared services - in
particular common patient data sets (e.g. name, address); applications and
application interfaces (e.g. authentication, payments, notifications); and core
ICT infrastructure.
·
use of the Internet
of Things to connect to
and use e-Devices including standards and common approaches for management of
the connections and security in line with patient choice and privacy
·
published
standards
to enable safe exchange of information between modules (all open, exportable,
and based wherever possible on international standards) and which cover: services;
data outcomes; rules; KPIs; interoperability.
·
a commitment
to enable both privacy and openness: all
personal data held securely, and under the ownership and control of the
individual patient; all non-personally identifiable public data open for reuse
and innovation by third parties;
·
tools
and resources: standards, metadata, tools, incentives and business
models to facilitate transition towards the blueprint architecture by
stakeholder organizations.
v v
v
The Solution
TGF programs should therefore work with stakeholders
(including government agencies, IT suppliers, SMEs and other delivery
partners) to establish and maintain an open, service-oriented, government-wide
IT architecture, and to develop a phased migration plan towards that
architecture, which:
- concentrates technology resources and efforts
around leveraging open standards and SOA Principles so as to ensure
development and deployment agility, and support all customer interactions,
from face-to-face interactions by frontline staff to online self-service
interactions.
- uses the Reference Model for Service-Oriented
Architecture [SOA-RM] as the primary
source for core concepts and definitions of the SOA paradigm realizes
discrete services that can perform work on behalf of other parties, with clear service descriptions and
contracts for any capability that is offered for use by another party.
- manages key ICT building blocks as
government-wide resources and make them available as re-usable, shared
services - in particular common customer data sets (e.g. name, address);
applications and application interfaces (e.g. authentication, payments,
notifications); and core ICT infrastructure.
·
wherever
possible prefers interoperable, open standards, particularly when these are
well supported in the market-place. Standards of particular relevance in this
context are:
·
OASIS Business Centric Methodology (BCM) Version 1.0.
·
OASIS Content Assembly Mechanism (CAM) Version 1.1.
·
EPR-forum e-Folder standard
·
EPR-forum e-Device standard
- pays due attention to the total cost of ownership
and operation of technology and consider the possible value of open source
when making technology choices.
v v v
Linkages
Shifting from the current set of legacy IT systems and
contractual arrangements to a more integrated, SOA-based approach that supports
e-Health in the Home and Community domain will be a multi-year process of
change. That process should be built in as a core element of the [B10]
Roadmap for Transformation and, in
particular, to work on [B7] Supplier Partnership (which is
essential in order to ensure that new procurements establish requirements and
supplier relationships that help build towards the future vision). And the
process will need proactive governance, as described in [T1] Digital Asset Mapping and
Management.
The European Interoperability Framework[EIF]
has a useful definition of “open” in 5.1.1 “Specifications, openness and
reuse”.
The TGF Core
Pattern [B6] sets out the requirement to use the Policy Product Matrix to
identify all the standards, policies, guidelines etc which are needed to make
sure all aspects of a cross-organization interoperability problem (political, legal,
organizational, semantic, technical,) are managed effectively. It also
advises that the Programme Leadership should undertake a policy gap analysis
through Engagement with Stakeholders, and then ensure that the accountability
and process for developing any missing Policy Products is embedded within the
Roadmap for Transformation.
Most of the TGF Policy Product Types
are relevant to the e-Health community. Some are very generic to all domains
of public sector activity and require no further explanation in this Profile. The
full text of them is available in the Matrix at https://wiki.oasis-open.org/tgf/Policy%20Products
However some are considered essential
for e-Health programmes and these are shown in full below suitably tailored for
that community.
6.1 Business Management
Layer
|
Policy
Product Type - TRANSFORMATIONAL OPERATING MODEL
|
|
Description:
The strategy for ensuring that the intended benefits from the e-Health
programme are delivered in practice.
|
|
|
Problem
Addressed: Target Business Operating Model
|
|
|
Example(s)
of current Policy Product of this type:
UK - http://digital.cabinetoffice.gov.uk/
|
|
|
Notes:
See TGF Pattern [B3] Transformational Operating Model as amended in this
Profile.
|
|
|
Policy
Product Type - LEGAL AUTHORITY FOR INTER-AGENCY COLLABORATION
|
|
|
Description: This represents the
legal basis for inter healthcare agency collaboration, data and information
exchanges and other joint activities.
|
|
|
Problem Addressed: An early step in
the Transformation Roadmap for many governments is the identification and
redressing of legal barriers. Very often existing laws and practices prohibit
full inter-agency working, for example by limiting the ability of an agency
to act for tightly prescribed purposes.
|
|
|
Example(s) of current Policy Product of this type:
None available
|
|
|
Notes: National legislation will vary
on this aspect so it will be necessary to consult with Government lawyers to
identify and remove any barriers.
See also:
EU - European Commission – Article 3 and Part III(c) §2 of Annex of the
Proposal for a Regulation establishing the Connecting Europe Facility http://europa.eu/rapid/pressReleasesAction.do?reference=IP/11/1200&format=HTML&aged=0&language=EN&guiLanguage=en
Scotland - eCare Data Transfer Guidance Note - http://www.scotland.gov.uk/Resource/Doc/1141/0110087.doc
UK - A guide to inter-agency working to safeguard the welfare of children - https://www.education.gov.uk/publications/eOrderingDownload/00305-2010DOM-EN-v3.pdf
|
|
6.1.3 “Business Management/Organisational”
|
Policy Product Type - COMMON TERMINOLOGY AND
REFERENCE MODEL
|
|
Description: The
means by which all stakeholders have a common understanding of the key
concepts involved in the e-Health programme and how they interrelate, and the
common language to describe them.
|
|
|
Problem Addressed:
Common Language
|
|
|
Example(s) of current Policy Product of this
type:
None available
|
|
|
Notes: See TGF
Pattern [B9] Common Terminology and Reference Model and the e-Health Glossary
in this Profile.
|
|
|
Policy
Product Type - BUSINESS PROCESS MODEL
|
|
Description:
A model that depicts the business processes of an organization or community.
The model typically shows a collection of related, structured activities or
tasks that produce a specific service or product for a particular patient or
set of patients. It often can be visualized with a flowchart as a sequence of
activities.
|
|
|
Problem
Addressed: Business Processes
|
|
|
Example(s)
of current Policy Product of this type:
USA Consolidated Reference Model - http://www.whitehouse.gov/omb/e-gov/fea
Zachman - http://www.zachman.com
|
|
|
Notes:
See TGF Pattern [T1] Digital Asset and Mapping Management
See also OMG's Business Process Model - http://www.omg.org/spec/BMM/
|
|
6.2 Service Management Layer
|
Policy
Product Type - PRIVACY AND DATA SHARING POLICY
|
|
Description: The government or
healthcare community policy for the sharing of data between practitioners,
whilst at the same time respecting the needs for data privacy of patients’
records.
|
|
|
Problem Addressed: Data Privacy and
Sharing
|
|
|
Example(s) of current Policy Product of this type:
EU European Commission, EIF v2 para 2.5 - http://ec.europa.eu/isa/policy/policy3_en.htm
|
|
|
Notes: See TGF Pattern [S3] Identity
and Privacy Management
|
|
|
Policy
Product Type - ACCCESSIBILITY GUIDELINES
|
|
Description: Guidelines setting out
how to make content available to all patients, particularly those with
disabilities, including visual, auditory, physical, speech, cognitive, and
neurological disabilities.
|
|
|
Problem Addressed: Accessibility
|
|
|
Example(s) of current Policy Product of this type:
Queensland Government - http://www.qld.gov.au/web/cue/
W3C Web Accessibility Initiative - http://www.w3.org/WAI/intro/components.php
|
|
|
Notes: See TGF Pattern [S4] Channel
Management Framework
|
|
6.2.3 “Service
Management/Technical”
|
Policy Product Type - SERVICE DEFINITION FOR ONE
STOP SERVICES
|
|
Description: e-Health programmes typically involve a shift from silo-based
delivery towards an integrated, multi-channel, patient centric service
delivery platform offering “one stop” service delivery and self-help for healthcare.
Developing such a service requires a clear end-to-end service definition: a
comprehensive documentation describing the product which will be offered to
all patients.
|
|
|
Problem
Addressed: One stop service delivery
|
|
|
Example(s)
of current Policy Product of this type: None
available
|
|
|
Notes: See TGF Pattern [B3] Transformational Operating Model as amended
in this Profile.
|
|
|
Policy Product Type - SINGLE SIGN-ON ARCHITECTURE
|
|
Description: The architecture that sets out how patients can access all the
services and self help facilities they require through a single sign-on
facility.
|
|
|
Problem
Addressed: Single sign-on
|
|
|
Example(s)
of current Policy Product of this type: None
available
|
|
|
Notes: See TGF Pattern [T2] Technology Development and Management as
amended in this Profile.
|
|
6.3
Technical and Digital Asset Management Layer
6.3.1 “Technical and Digital Asset Management/Political”
6.3.2 “Technical
and Digital Asset Management/Organizational”
|
Policy Product Type - APPLICATIONS ARCHITECTURE
|
|
Description: An architecture that
sets out how a suite of applications are being used by the e-Health programme
to create a composite application that is scalable, reliable, available and
manageable. It is specified on the basis of business and functional
requirements.
|
|
|
Problem Addressed: IT Management
|
|
|
Example(s) of current Policy Product of this type:
Zachman - http://www.zachman.com
|
|
|
Notes: See TGF Pattern [T2]
Technology Development and Management as amended in this Profile.
|
|
|
Policy Product Type - NETWORK ARCHITECTURE
|
|
Description: An architecture showing
the design of the communications network for the e-Health programme. Usually
the Internet would be used as the network but if an alternative is used then
there is the need for the specification of the network's physical components
and their functional organization and configuration, its operational
principles and procedures, as well as data formats used in its operation.
|
|
|
Problem Addressed: Network Management
|
|
|
Example(s) of current Policy Product of this type:
Zachman - http://www.zachman.com
|
|
|
Notes: See TGF Pattern [T2]
Technology Development and Management as amended in this Profile.
|
|
The following individuals have participated in the creation
of this specification and are gratefully acknowledged:
Participants:
Hans A Kielland Aanesen, Individual Member
John Borras, Individual Member
Peter F Brown, Individual Member
Geoff Clarke, Microsoft Corporation
Nig Greenaway, Fujitsu Ltd
Gershon Janssen, Individual Member
Chris Parker, CS Transform Ltd
Colin Wallis, New Zealand Government
Joe Wheeler, MTG Management Consultants, LLC
In addition we acknowledge the contributions from
the OASIS BCM and CAM Technical Committees.
|
Revision
|
Date
|
Editor(s)
|
Changes Made
|
|
01
|
4 March 2015
|
Hans A.
Kielland Aanesen
John Borras
|
Initial draft
|
|
02
|
19 March 2015
|
Hans A.
Kielland Aanesen
John
Borras
|
Draft approved by TC for Public Review
|
![]()