![]()
Transformational Government Framework e-Health Profile Version 1.0
Committee Note 01
19 June 2014
Specification URIs
This version:
http://docs.oasis-open.org/tgf/TGF-eHealth-Profile/v1.0/cn01/TGF-eHealth-Profile-v1.0-cn01.pdf (Authoritative)
http://docs.oasis-open.org/tgf/TGF-eHealth-Profile/v1.0/cn01/TGF-eHealth-Profile-v1.0-cn01.html
http://docs.oasis-open.org/tgf/TGF-eHealth-Profile/v1.0/cn01/TGF-eHealth-Profile-v1.0-cn01.doc
Previous version:
N/A
Latest version:
http://docs.oasis-open.org/tgf/TGF-eHealth-Profile/v1.0/TGF-eHealth-Profile-v1.0.pdf (Authoritative)
http://docs.oasis-open.org/tgf/TGF-eHealth-Profile/v1.0/TGF-eHealth-Profile-v1.0.html
http://docs.oasis-open.org/tgf/TGF-eHealth-Profile/v1.0/TGF-eHealth-Profile-v1.0.doc
Technical Committee:
OASIS Transformational Government Framework TC
Chair:
John Borras (johnaborras@yahoo.co.uk), Individual
Editors:
John Borras (johnaborras@yahoo.co.uk), Individual
Hans A. Kielland Aanesen (hans@eprforum.no), Individual
Nig Greenaway (nig.greenaway@uk.fujitsu.com), Fujitsu Ltd.
Related work:
Abstract:
This Committee Note contains detailed information and guidance on using the Transformational Government Framework (TGF) and other OASIS standards to support the work of the delivery of e-Health services provided in the home or in the community. It identifies in particular which of the Core Patterns and Policy Products are relevant and where necessary elaborates them more specifically to the e-Health domain.
By applying the principles and good practices of the TGF to the setting up and management of e-Health programmes, all stakeholders should be able to deliver a more effective and efficient response to the future needs of patients and healthcare practitioners.
Further guidance on any aspects can be obtained from the TGF Technical Committee using the “Send A Comment” button on the TC’s web page.
Status:
This document was last revised or approved by the OASIS Transformational Government Framework TC on the above date. The level of approval is also listed above. Check the “Latest version” location noted above for possible later revisions of this document.
Technical Committee members should send comments on this document to the Technical Committee’s email list. Others should send comments to the Technical Committee by using the “Send A Comment” button on the Technical Committee’s web page at https://www.oasis-open.org/committees/tgf/.
Citation format:
When referencing this document the following citation format should be used:
[TGF-eHealth-v1.0]
Transformational Government Framework e-Health Profile Version 1.0. Edited by John Borras, Hans A. Kielland Aanesen, and Nig Greenaway. 19 June 2014. OASIS Committee Note 01. http://docs.oasis-open.org/tgf/TGF-eHealth-Profile/v1.0/cn01/TGF-eHealth-Profile-v1.0-cn01.html. Latest version: http://docs.oasis-open.org/tgf/TGF-eHealth-Profile/v1.0/TGF-eHealth-Profile-v1.0.html.
Copyright © OASIS Open 2014. All Rights Reserved.
All capitalized terms in the following text have the meanings assigned to them in the OASIS Intellectual Property Rights Policy (the "OASIS IPR Policy"). The full Policy may be found at the OASIS website.
This document and translations of it may be copied and furnished to others, and derivative works that comment on or otherwise explain it or assist in its implementation may be prepared, copied, published, and distributed, in whole or in part, without restriction of any kind, provided that the above copyright notice and this section are included on all such copies and derivative works. However, this document itself may not be modified in any way, including by removing the copyright notice or references to OASIS, except as needed for the purpose of developing any document or deliverable produced by an OASIS Technical Committee (in which case the rules applicable to copyrights, as set forth in the OASIS IPR Policy, must be followed) or as required to translate it into languages other than English.
The limited permissions granted above are perpetual and will not be revoked by OASIS or its successors or assigns.
This document and the information contained herein is provided on an "AS IS" basis and OASIS DISCLAIMS ALL WARRANTIES, EXPRESS OR IMPLIED, INCLUDING BUT NOT LIMITED TO ANY WARRANTY THAT THE USE OF THE INFORMATION HEREIN WILL NOT INFRINGE ANY OWNERSHIP RIGHTS OR ANY IMPLIED WARRANTIES OF MERCHANTABILITY OR FITNESS FOR A PARTICULAR PURPOSE.
Table of Contents
1.1 References (non-normative)
4 Implementing the New Service Model
4.1 National Transformational Infrastructures
4.5 The Use of OASIS Standards
4.5.1 Transformational Government Framework (TGF)
4.5.2 Business-Centric Methodology (BCM)
4.5.3 Content Assembly Mechanism (CAM)
5.1 Core Pattern B1 - Vision for Transformation
5.2 Core Pattern B3 -Transformational Operating Model
5.3 Core Pattern B7 –Stakeholder Collaboration
5.4 Core Pattern B9 - Common Terminology and Reference Model
5.5 Core Pattern T2 - Technology Development and Management
6 e-Health Policy Product Types
6.1.1 “Business Management/Political”
6.1.2 “Business Management/Legal”
6.1.3 “Business Management/Organisational”
6.1.4 “Business Management/Semantic”
6.2.1 “Service Management/Political”
6.2.2 “Service Management/Semantic”
6.2.3 “Service Management/Technical”
6.3 Technical and Digital Asset Management Layer.
6.3.1 “Technical and Digital Asset Management/Political”
6.3.2 “Technical and Digital Asset Management/Organizational”
6.3.3 “Technical and Digital Asset Management/Technical”
The delivery of health services around the world is changing rapidly, brought about by advances in surgical and non-surgical treatments, the increasing aged population, funding pressures, and the increased availability of self-help facilities and private healthcare schemes. Less time is being spent in hospitals through advances in surgery recovery times, pressures on beds, the availability of better home help services, etc. This all requires a new model of the delivery of health services provided in the home or in the community, ie not primary or secondary care services provided in hospitals and doctors’ surgeries.
For the purposes of this profile it is necessary to differentiate between what is commonly called primary and secondary care, and home and community care. Primary care refers to the work of healthcare professionals who act as a first point of consultation for all patients within a healthcare system, and secondary care is the healthcare services provided by medical specialists and other health professionals who generally do not have first contact with patients. Home and community care refers to the many types of healthcare interventions delivered outside of these primary and secondary facilities. It includes the services of professionals in residential and community settings in support of self care, home care, long-term care, assisted living, and treatment for substance use disorders and other types of health and social care services.
This profile focuses on the latter category and describes how these future home and community services can be delivered using new disruptive and interacting technologies and using open standards developed by OASIS and other organizations.
Remote Healthcare is just one facet of life that is made possible by the Internet of Things (IoT) [Ref 11]. The IoT integrates physical objects into information networks and allows those physical objects to become active participants in business processes. This provides a basis for devices to monitor patients’ health, track and record exercise, sleep, and health information and to tell practitioners whether treatment is being applied, and if so, how it’s working.
1.1 References (non-normative)
[Ref 1] Diagrams of e-Devices and other self-care facilities see http://www.eprforum.no
[Ref 2] e-Device apps developed in USA see http://video.msnbc.msn.com/rock-center/50582822#50582822.
[Ref 3] Technical University of Munich (TUM) research see http://www.tum.de/en/about-tum/news/press-releases/short/article/30440/
[Ref 4] Edinburgh University research see http://www.bbc.co.uk/news/uk-scotland-22695278
[Ref 5] Public Supervision & Quality Assurance (PSQA) see http://www.eprforum.no/product.php/Supervision-and-Quality-in-Home-care-services/50/
[Ref 6] e-Folder standard see http://www.eprforum.no/product.php/Standard-EPR-and-e-Folder/3/
[Ref 7] e-Device standard see http://www.eprforum.no/description.php/EPR-eDevice/5/
[Ref 8] OASIS BCM-EPR SC see https://www.oasis-open.org/committees/tc_home.php?wg_abbrev=bcm-epr
[Ref 9] CAM templates see http://www.eprforum.no/product.php/CAM-Template-EditorProcessor/37
[Ref 10] European Interoperability Framework (EIF) version 2.0 see http://ec.europa.eu/isa/documents/isa_annex_ii_eif_en.pdf
[Ref 11] The Internet of Things see http://en.wikipedia.org/wiki/Internet_of_Things
2 The e-Health TGF Profile
The Profile contained in this Committee Note contains detailed information and guidance on using the TGF and other OASIS standards to support the work of the home and community healthcare community. A full explanation of the TGF is given in the TGF v2.0 and whilst this Committee Note makes no attempt to re-write that document, it does “translate” the most relevant parts into the language more appropriate for that community. It also identifies in particular which of the Core Patterns and Policy Products are relevant and where necessary elaborates them more specifically to the healthcare domain.
The Transformational Government Framework is a practical “how to” standard for the design and implementation of an effective programme of technology-enabled change at national, state, county or local government level. It sets out a managed process of ICT-enabled change in the public sector, which puts the needs of citizens and businesses at the heart of that process and which achieves significant and transformational impacts on the efficiency and effectiveness of government. The Framework is applicable to a variety of domains of government activity and although the TGF talks primarily about the delivery of citizen-centric services it is equally applicable to other areas of public sector business including healthcare in the home and community. The fundamental principles being that the structures, governance, funding, culture, and stakeholder engagement are all organized in a holistic way for the benefit of patients and healthcare practitioners, which has to be the primary objective of any e-Health programme.
The TGF makes the point that all around the world, governments at national, state, and local levels face huge pressure to do “more with less” and every government faces the challenge of achieving their policy goals in a climate of increasing public expenditure restrictions. This situation is equally true for those responsible for operating e-Health programmes and there are clear opportunities to realize economic benefits through full citizen, business and private sector stakeholder engagement in the development of home and community healthcare programmes.
Advances in technology, such as the Internet of Things, are providing the devices and means of delivering necessary healthcare services to locations away from hospitals and surgeries, eg to patients’ homes, care homes, holiday homes, etc. Through the use of these various devices and also online self-help facilities [Ref 1] patients can service their own needs but at the same time trigger emergency help when the need arises. The new disruptive technologies available today are helping to create new markets and value networks, and displacing earlier technologies. This includes handling health condition monitoring in real time enabling actions to be taken before emergency help and resources are needed.
Use of these technologies and devices does not take away the need for face-to-face interaction but they do enable that time commitment can be kept to a minimum and thus reduce the burdens on the already over-stretched healthcare resources. It also enables the desire of many patients today, especially the elderly, to be independent and remain in their own homes rather than being kept in hospital or in care homes.
Examples of the advances being made are as follows:
- doctors in USA [Ref 2] have developed a number of apps that can run on a smart phone providing remote, wireless diagnosis and monitoring that can lead to better and cheaper healthcare and provide lifestyle changes for the patient . They are also developing a remote wireless monitor that can be worn on the wrist to reduce the need for constant visits to a hospital or surgery.
- researchers at the Technical University of Munich (TUM) [Ref 3], in collaboration with business partners, have designed an assistive system for helping senior citizens live at home by embedding a tablet computer in the wall. As well as providing a central location where users can access all of the information they need, such as family and emergency phone numbers, it also contains biosensors that can measure vital signs so the system can recommend exercise or medication, or alert a physician or mobile nursing service if the health problem is critical.
- researchers at Edinburgh University [Ref 4] found that the blood pressure of people who used a self-monitoring system in a six-month trial dropped further than those who did not. A portable machine which lets people measure their own blood pressure and send results directly to doctors is said to have improved patient health. The portable system allowed patients to send readings to doctors and nurses, who then checked the figures and, if necessary, contacted the patient to discuss their health and medication.
Whilst the technology exists today as these examples demonstrate, there is a need to ensure that all the various devices can work together and provide a single view of the patient’s care needs. Aspects such as patient choice and privacy must also be considered. That is where the use of standards comes in and it requires hardware and software providers to use these standards to ensure there is the necessary interoperability that enables the required flows of data between patients and healthcare practitioners.
In addition to making the various devices work together, huge benefits can be achieved with a single system of data entry - as more and more people are being discharged from hospitals sooner, with more focus on management in the community, having that vital information about what has been happening in either sector provides a more effective prompt service to the patient. Much time is wasted in hospital in trying to find out what has been happening in the community before admission, and vice-versa, so if this information is readily available, more productive time can be spent ensuring the patient gets the required treatment. And it promotes better multi-disciplinary working if all health professional notes are shared, because each professional's work is affected by another’s. Linking these various records is valuable to monitor those patients who are at risk of self neglect or isolation in the community, subject to patient choice and privacy constraints.
There are a number of aspects that need to be addressed in order to implement the new service model for home and community healthcare. These are described in the following sub-sections.
4.1 National Transformational Infrastructures
Dealing with global Internet information exchanges on a large number of different world based connected national infrastructures requires the need to split the global governance of the physical infrastructures and the private and public controlled services running on them. Cloud technology should not exclusively be controlled by private business enterprises; they need to co-operate with public cloud services and be subject to quality standards (for example, the Norwegian Public Supervision & Quality Assurance (PSQA) [Ref 5] approach). Cloud services should show a clear split between the data and the software solutions. The data should be preserved for “ever” but the software needs to be substituted and changed according to the technology development. Today several national governments are wasting enormous amounts of money on infrastructures run on private software vendor’s regimes. Adaptive and agile templating requires a clear split between shared data and the different interacting software applications.
Ineffective and inefficient progress can be seen in many countries where taxpayers’ money is being wasted building unneeded isolated public networks with tied up services not available for the citizens or other application business areas such as:
- Healthcare networks
- Smart Grid networks
- Police networks
- Military networks
- Emergency networks
- Broadcasting networks
- Tax system networks
- Road and Railroad control networks
- etc
However, it is important to realize that ‘one size fits all’ is not usually a valid approach. For example, low-power free-to-use alternatives may be appropriate for linking e-Devices where there are small amounts of data to transfer, where battery life is an issue, and where network charges would make the application uneconomic.
New thinking is required to differentiate between the following 5 important related aspects:
1. National communication infrastructures - "Information Highways" the national physical interacting packet switched IP-networks using basically Fibre and 4G-mobile networks.
- Shared Data - shared persistent data in public registers.
- Abstract Common and Open Service Models handling Information Exchange - downward semantic compatibility interacting on the shared data.
- Traditional Software programmes/platforms - the software should be adapted and substituted continuously according to new applications, legislations, technology and methodologies. All information exchange should be done through common certificated Service Models.
- Executing legislated public services and buying care equipment - undertaken by both private and public enterprises.
Today’s typical mix of these 5 areas into silo and monopolistic systems of locked vendor regimes do prevent the needed interaction reforms in public sector to succeed, especially regarding the often legislated public services needing a common national interaction area indicated by 1, 2 and 3 above. This has to do with society’s backbone responsibility of administrations tasks, not driven by profit goals, but operating securely and enabling fair competition in areas 4 and 5 above for business related software and attached services. Even if areas 1-3 are the public sector’s responsibility, companies should be able to compete on common terms to handle them, but these companies should be prevented from delivering software programmes/platforms or services to avoid a monopolistic or oligopolistic market situation.
4.2 Service Management
The physical implementation of this new service model will be by using the Internet to enable standardized flows of data between patients and the executers of healthcare services. Most of this data comes directly from the patient’s own monitoring e-devices but also via self-help facilities. Through a neutral and public defined “Super Structure” it is possible to demonstrate how to solve much of the rising healthcare interaction problems related to the holistic approach of needed common information exchange modelling. The interaction via the Internet enables new ways of self diagnosis, self service and use of expertise through new ways of frontline service management as covered in the TGF.
One way of implementing this new agile meta-engineering is through the use of the Norwegian EPR Public Supervision and Quality Assurance programme ( PSQA ) [Ref 5] which is developing a common electronic framework for the healthcare supervision and quality assurance of citizen services and for the business enterprises involved.
PSQA is intended to be used
in all relevant healthcare supervisions and by the enterprises that need to
comply with the supervision requirements. It is based on international quality
standards and uses electronic folders that integrate and interact with the
underlying legacy and expert systems in general handling the service
management.
An important aspect is the
interaction between the workflow service management for service executers
dealing with the e-Folders [Ref 6] and
the condition monitoring and deviation response system handled by e-Devices [Ref 7] in real-time, home automation and body sensing
condition monitoring. Typical application areas are:
· Integrated e-Device Condition monitoring ( Body and Environment adapted User Scenarios)
· Interaction of e-Folder Service work, Planning and Reporting (task description, reporting and inspection)
· Service Tools access using the OASIS CAM Templating editor (role control by digital signature using the OASIS PKI standard )
4.3 The Use of e-Folders
The solution to delivering the service management described above is to extract the computer support into electronic folders. The folders have a standard design with standardized functionality and give the user access to all needed information and help in the performance of the task. Access is given through "single sign on" and approved digital signatures for identification. Special applications and expert systems can be integrated into the folders.
Important properties of the use of e-folders being introduced in Norway are:
· The folders are a framework. The framework has several purposes, a common access point for all relevant information, in order to integrate under laying systems, to be used as next generation of “front office". The framework will function by use of open standards for processing XML-based templates. The folders will also be able to use a number of other standards.
· Integration of applications and data will be controlled by commands (on demand). Applications can be components in special applications, expert systems, and help for users e.g. access on command is the opposite of permanent access. Access on command belongs to a technology called loosely-coupled applications.
· The folders are customized (adapted) for the actual need. This means that only correct and needed information will be available through the folders.
· The folders are dynamic; they can be extended or reduced as needed. This is possible because of the standardized structure that the folders have been designed around. The structure is the base for automatic modeling of generic information.
The principles around customized folders and access on command are important components in order to avoid unnecessary dispersion of information. In addition to clear role structure this is especially important in order to protect sensitive information and to protect personal integrity.
4.4 The Use of e-Devices
|
|
Environmental control and patient condition monitoring through interoperating electronic equipment is crucial for self-centric healthcare management. Work is ongoing within the OASIS BCM-EPR Sub-Committee [Ref 8] to produce a functional standard for e-Devices. The standard sets down the Methodology for Condition Monitoring and the environmental access control template management. It represents a standardized functional mirrored model of electronic network devices (nodes) that are connected to e-Folders content through Web services technology. It is derived from the ANSI/CEA-721 work developed over the last 25 years by more than 400 companies, organizations and individuals. The standard demonstrates how all the real open BUS-technology standards can interact through a common top level real open XML based functional modelling layer.
4.5 The Use of OASIS Standards
Many of the standards required to support the delivery of the services described above have been developed by OASIS. The three described below provide the means of defining and developing the specific model for the home and community service care.
4.5.1 Transformational Government Framework (TGF)
The most relevant characteristics of the TGF approach that support this new healthcare service model are:
· it takes a whole-of-government view of the relationship between the public sector and the citizen. This provides the correct working environment for the new service model to be developed through the use of joined-up resources across agencies, the sharing of data, the use of common rules and procedures, etc.
· it recognizes the need to e-enable the whole frontline of public services: that is, including staff and organizations involved in direct, personal delivery of services (such as healthcare) as well as e-enabling transaction-based services.
Using the TGF approach will ensure an effective programme of change can be developed to deliver the services for the new home and community care model. It will ensure that all the necessary stakeholders are involved, that resources are correctly identified and managed, and that the envisaged benefits and outcomes are achieved.
4.5.2 Business-Centric Methodology (BCM)
The Business-Centric Methodology is a specification that provides business managers with a set of clearly defined methods with which to acquire agile and interoperable e-business information systems within communities of interests. It provides managers with a clear understanding of what the business goals and appropriate steps are that need to be applied for a specific project to succeed.
The BCM efforts are on communication at three levels: (1) lexical, (2) semantic, and (3) pragmatic interoperability for sets of Community of Interest (CoI), eg healthcare. The BCM templates collect objectives and rationale for pragmatic interoperability by recording and sharing design decisions along with artifact data. The layered BCM products relate one or more artifacts together by including rich metadata on each link for semantic interoperability. The BCM combines together these components and calls for their management within an information architecture founded on conceptual agreements (lexical).
4.5.3 Content Assembly Mechanism (CAM)
The Content Assembly Mechanism specification provides a generalized assembly mechanism using templates of business transaction content and the associated rules. Information exchanges are moving to technical formats using XML technology worldwide. However XML by itself is only a mark-up language, it was never intended to support exacting business interchange definitions, rules and industry vocabularies. To provide that extra level of robust information definition and exact control CAM has been developed to enable business users to quickly and easily use templates to declaratively assert these missing business rules and structural information requirements.
Working examples [Ref 9] using the CAM editor have been developed to make the necessary template models for 3 e-Device health units, a SmartGrid Light sensor, a Thermostat and an Electrical meter, and more are being developed.
The Transformational Government Framework (TGF) Standard is expressed as a series of Core Patterns. The rationale for using the Pattern Language approach and the format of them is set out in the TGF v2.0 document and that should be read in conjunction with this Section.
Most if not all of the TGF Core Patterns are relevant to the healthcare community. Some are very generic to all domains of government activity and therefore require no further explanation in this Profile. The full text of them is available in the TGF v2.0 document. However some are considered essential for e-Health programmes and these are shown in full below suitably tailored for that community but include references to the main TGF Core Patterns.
5.1 Core Pattern B1 - Vision for Transformation
Context
First among the [GP1] Guiding Principles is the need for [B2] Program Leadership to develop a clear, compelling and shared vision for the e-Health transformation program.
v v v
The Problem
Without a well-expressed vision, developed and bought into by all of the stakeholders, an e-Health transformation program is likely to become a disjointed set of initiatives and be dominated by technology issues.
It is not the intent of the Transformational Government Framework to describe some perfect “end-state” for governments and healthcare communities. All communities are different: the historical, cultural, political, economic, social and demographic context within which each operates is different, as is the legacy of business processes and technology implementation from which it starts. So the Transformational Government Framework is not a “one-size-fits-all” prescription for what a healthcare community should look like in future.
Rather, each e-Health program needs to set its own clear vision. This will require agreement and clarity amongst stakeholders on:
· the social, economic and/or environmental impacts that the program seeks to achieve;
· the challenges that an e-Health program needs to overcome in order to deliver these impacts and the vision should address – such as, for example:
− Healthcare budget pressures
− Changing patient needs
− Patient choice
− Patient privacy
− Advances in surgical and non-surgical treatments
− Infrastructure stress
− Resource scarcity
− Skills and market access
− Growing population
− Aging population
− Mobile population
− Economic inequality
− Digital divide
· how the future will “feel” different for key stakeholders – so that the vision is articulated not in technical terms, but also in human and emotional ones.
v v v
The Solution
Program Leadership must create a vision for the e-Health program that:
a) is developed in an iterative and collaborative manner (that is, inclusive of all stakeholder groups and informed by patient and practitioners research and engagement, with social media and other technologies used to enable wide public participation in the process);
b) embraces the opportunities opened up by new technologies and delivery channels, open data and effective collaboration;
c) does so in a way which integrates these with the core socio-economic, political and environmental vision for the future, rather than seeing them as somehow separate from the healthcare management’s core strategic objectives;
d) can be measured.
v v v
Linkages
The vision should be informed by the TGF program’s [GP1] Guiding Principles, and developed through intensive [B5] Stakeholder Collaboration. It is vital to ensure that the vision can be expressed in terms of measurable outcomes and that clear “line of sight” is established between all activities in the roadmap and delivery of these outcomes for the program vision. Guidance on how to do this effectively is set out at TGF v2.0 Section 7 Benefit Realization.
5.2 Core Pattern B3 -Transformational Operating Model
Context
A central task of the [B2] Program Leadership and [B5] Stakeholder Collaboration is to enable the machinery of government to deliver customer-centric services. The principles set out in that Pattern apply equally to the leadership of the e-Health programme and the delivery of care and services to patients. They need to cooperate with all stakeholders in developing a new business model that delivers that care and other services in practice, when and where they are needed.
v v v
The Problem
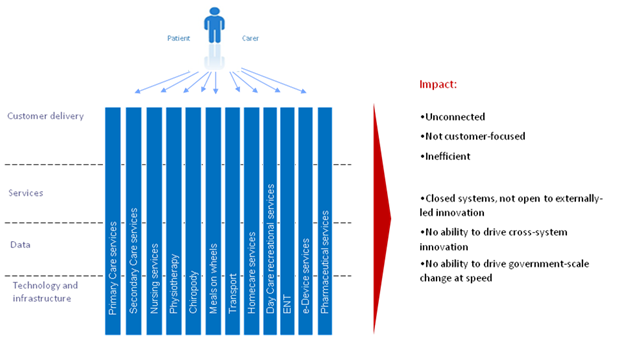
The failure to create an appropriate new operating model has arguably been the greatest weakness of most traditional healthcare programs. The transition to e‑Health has involved overlaying technology onto the existing operating model of the health care sector: an operating model based around existing functionally-oriented departments, agencies and practitioners. These behave like unconnected silos in which policy-making, budgets, accountability, decision-making and service delivery are all embedded within a vertically-integrated delivery chain based around delivery functions rather than patient needs.
The experience of healthcare communities around the world over the last two decades has been that silo-based delivery of services simply does not provide an effective and efficient approach to e-Health. Many attempts have been made to introduce greater cross-community coordination, but largely these have been "bolted on" to the underlying business model, and hence experience only limited success. Without examination of, or fundamental change to, the underlying business model level, the design and delivery of care and services remains fragmented and driven by the structures of the community, rather than the needs of the patients.
Figure 3 below illustrates the traditional operating model which is still typical of most governments and healthcare communities:
· the individual patient usually has to engage separately with each silo: making connections for themselves, rather than receiving seamless and connected service that meets their needs;
· data and information has typically been locked within these silos, limiting the potential for collaboration and innovation across the community, and limiting the potential to drive change at speed.
|
|
|
|
Figure 3 – Traditional operating model: where healthcare communities have come from
Healthcare transformation programs involve a shift in emphasis, away from silo-based delivery and towards an integrated, multi-channel, service delivery approach: an approach which enables a whole-of-community view of the patient and an ability to deliver services to patients where and when they need it most, including through one-stop services and through private and voluntary sector intermediaries.
Key features of this shift to a transformational operating model include:
a) investing in smart data, i.e. ensuring that data on the performance and use of the healthcare community’s physical, spatial and digital assets is available in real time and on an open and interoperable basis, in order to enable real-time integration and optimization of resources;
b) managing public sector data as an asset in its own right, both within the community and in collaboration with other significant data owners engaged in the e-Health program;
c) enabling externally-driven, stakeholder-led innovation by patients, carers, communities and the private and voluntary sectors, by opening up data and services for the common good:
· both at a technical level, through development of open data platforms;
· and at a business level, through steps to enable a thriving market in reuse of public data together with release of data from commercial entities in a commercially appropriate way;
d) enabling internally-driven, practitioner-led innovation to deliver more sustainable and patient-centric services, by:
· providing patients with healthcare and services, which are accessible in one stop, over multiple channels, that engage patients, carers, specialists and communities directly in the creation of services, and that are built around patient needs not the healthcare community’s organizational structures;
· establishing an integrated business and information architecture which enables a whole-of-health service domain view of specific patient groups for e-Health services (e.g. elderly people, drivers, parents, disabled people);
e) setting holistic and flexible budgets, with a focus on value for money beyond standard departmental boundaries;
f) establishing community-wide governance and stakeholder management processes to support and evaluate these changes.
Figure 4 summarizes these changes to the traditional way of operating which transformational healthcare programs are seeking to implement.
|
|
Figure 4 – New integrated operating model: where healthcare communities are moving to
v v v
The Solution
e-Health programs should therefore ensure that their [B1] Vision for Transformation includes the need to establish a Transformational Operating Model to help build healthcare services around patient needs, not just healthcare community’s organizational structure. This will include:
- providing patients with healthcare and services which are accessible via a common point or contact (generally a specialist) and ideally offered over multiple channels, where appropriate;
- enabling those services also to be delivered by private and voluntary sector intermediaries.
The Transformational Operating Model must go beyond simple coordination between the existing silos and should include:
- An integrated business and information architecture which enables a whole-of-patient view, thus making possible both the integration of services and simple, effective cross-organizational patient journeys;
- Incentives and business processes that encourage the internal cultural change and cross-silo collaboration needed to drive the integration and joining-up of services;
- A cross-community strategy for shared development, management and re-use of common patient data sets, applications, and applications interfaces (e.g. authentication, payments, and notifications);
- Opening up public data for re-use and innovation by the private and voluntary sectors, and directly by patients.
v v v
Linkages
Rather than attempting to restructure healthcare communities to deliver such a Transformational Business Model, the [B4] Franchise Marketplace SHOULD be considered as the recommended approach to implement this model. Multi-channel delivery of services can be provided through optimized [S6] Channel Transformation and public data can be opened up to create new sorts of value through [S1] Stakeholder Empowerment. Common patient data sets can be built as shared services with customer data under customer control and managed using [T2] Technology Development and Management. This pattern is facilitated by placing patient and organizational data under their control as set out in [S3] Identity and Privacy Management.
5.3 Core Pattern B7 –Stakeholder Collaboration
Context
Effective stakeholder collaboration is critical. Establishing a process of sustainable change requires a critical mass of actors inside and outside of the Home and Community practitioners to be both engaged and supportive. Delivering a [B1] Vision for Transformation cannot be done without meaningful stakeholder collaboration.
The public, private, voluntary and community healthcare sectors have considerable influence on patients’ attitudes and behavior. These influences must be transformed into partnerships which enable the market to deliver programme objectives. This requires a “map” of all stakeholders as part of overall business management.
v v v
The Problem
It is not enough to map and understand stakeholder relationships and concerns. Classic models of stakeholder engagement also need to be re-assessed.
Leaders from all parts of the health organization, as well as other organizations involved in the program, need to be motivated for the program to succeed and need to be engaged in clear and collaborative governance mechanisms to manage any risks and issues. The development and delivery of an effective e-Health program requires engagement with a very wide range of stakeholders, not only across the whole of government but also, in most cases, with one or more of the private, voluntary and community healthcare sectors as well as with patients and other service customers. A significant effort is needed to include all stakeholders in the governance of the e-Health program at an appropriate and effective level.
Key elements are set out below that a conformant e-Health program will need to address in developing its Collaborative Stakeholder Governance Model, if it is to engage successfully with stakeholders and align them effectively behind shared objectives.
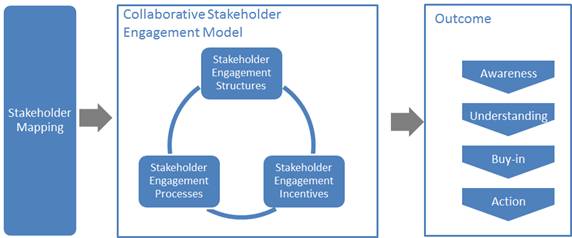
Figure 6: Overview of Collaborative Stakeholder Governance
It is vital to describe and map the complete landscape of relevant stakeholders. The Transformational Government Framework puts the individual – whether acting on their own behalf as a citizen or on behalf of another citizen or of a business– at the centre:
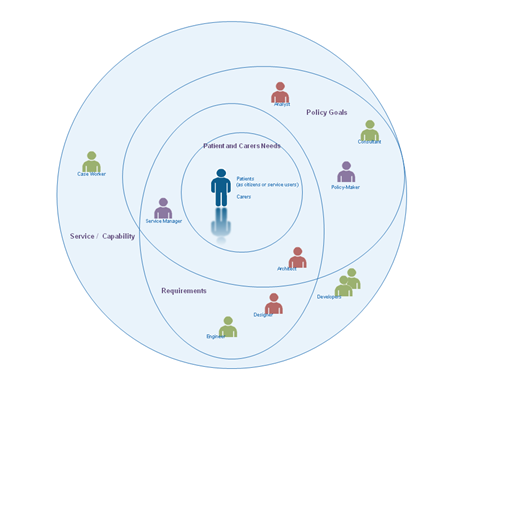
Figure 7: Landscape of some key stakeholders
This view deliberately and completely avoids the rather generic concept of ‘User’ that is dominant in traditional IT stakeholder engagement models, preferring rather to identify the different interests and concerns that are at stake (the mauve labels) and the key groups of stakeholders (the different people icons) in the development of any service.
The figure is by no means complete nor the only ‘valid’ view. It seeks instead to illustrate that the process of transformation requires reappraisal of the current set-up and assessment of what needs to change.
By clearly separating out key stakeholder groups and starting to understand and articulate their specific concerns as stakeholders (any individual’s role may vary according to context: in one situation, a person is a parent; in another, a policy-maker; or another, a service provider), we can start to understand how stakeholders relate (in different roles): to each other; to various administrations and services involved; to policy drivers and constraints; and how these all come together in a coherent ecosystem supported by a Transformational Government Framework. In this view:
A service (or ICT capability made available as a service) is understood as responding to a set of requirements and policy goals (some of which overlap) – stakeholders concerned at this level include, for example, case workers in a public administration or developers who have worked with them in delivering a specific service;
Requirements encapsulate and formalize vaguely stated goals and needs of patients, carers and businesses and take on board the policy goals of the political sponsor or champion – stakeholders at this level include, for example, managers of public service who can articulate the needs of their respective services, the information and systems architects who capture those needs as formal requirements that engineers can work with to develop services;
Policy Goals capture the high-level concerns and priorities of the political and health authorities and continually assess how these goals reflect key patient and service delivery concerns – stakeholders include policy makers and senior management as well as consultants and analysts involved in helping identify technology and administrative trends that can be used to leverage those goals; and finally;
Patient, carer and specialist needs that, ultimately, can only be fully understood by the people concerned themselves – nonetheless stakeholders at this level can also include patient or business associations, consumer and other interest groups who engage with policy makers to advance the interests of certain groups with distinct needs and are able to articulate those needs in ways that can be used by analysts and consultants.
The various ellipses in the diagram above are deliberately not concentric circles. This is to underline that the process of establishing a service or capability is not a linear one going from needs, goals and requirements. In reality stages are often inter-related.
The mapping of stakeholders and their principal concerns at a generic level is used as a key input to the TGF [B9] Reference Model and that needs to be validated within any e-Health program. It is valuable as a tool for encouraging collaborative governance as it renders explicit many of the relationships and concerns that are often left implicit but nonetheless impact on an organization’s ability to reflect stakeholders’ concerns.
However, it is not enough simply to map and understand stakeholder relationships and concerns. An effective e-Health program will also address the three other dimensions of the model illustrated above:
Stakeholder Engagement Structures: the organizational arrangements put in place to lead the transformation program, e.g.:
- central unit(s)
- governance boards
- health communities.
Stakeholder Engagement Processes: the processes and work flows through which the e-Health Leadership and the different Stakeholders interact, e.g.:
- reporting and accountability processes
- risk management processes
- issue escalation processes
- consultation processes
- collaborative product development processes.
Stakeholder Incentives: the set of levers available to drive change through these governance structures and processes. These will vary by jurisdiction, but typical levers being deployed include:
- central mandates
- political leadership
- administrative championship
- personal performance incentives for healthcare professionals
- alignment between public policy objectives and the commercial objectives of private sector partners.
There is no one right model for doing this successfully, but any conformant e-Health program needs to make sure that it has used the framework above to define its own Collaborative Stakeholder Engagement Model which explicitly articulates all of these elements: a comprehensive stakeholder map, coupled with the structures, processes and incentives needed to deliver full understanding and buy-in to the program, plus effective stakeholder action in support of it.
Collaboration between e-Health Programs
The model clearly focuses attention within any specific e-Health program. However (and increasingly) collaboration is required also between governments and healthcare communities and, by implication, between e-Health programs. In the figure below, we see that collaboration between e-Health programs is favoured at the political, legal and organizational levels and only later, if and when necessary, at the more ‘tightly-coupled’ semantic and technical levels.

Figure 8: Collaboration between eHealth programs through different levels of Interoperability
This approach is also consistent with the SOA paradigm for service development – not only are requirements defined and services offered independently of any underlying technology or infrastructure but also one e-Health program can be seen (and may need to be seen) as a ‘service provider’ to another e-Health program’s ‘service request’. For example, a patient wishing to use healthcare facilities in a second country may need to provide authenticated information and credentials managed by the government or health care community in the first country.
A further advantage of this approach is that it becomes easier to identify and manage high level government requirements for services: whether in the choice of ICT standards that may need to be used to address a particular technology issue or determining the criteria for awarding public procurement contracts, this approach allows a ‘loose-coupling’ at the level of clearly defined high-level policy needs rather than the more tightly-coupled and often brittle approach of specifying particular technologies, software or systems.
v v v
The Solution
e-Health programs should establish, and give high priority and adequate resources to, a formal managed stakeholder engagement program. This should be led by a senior executive and integrated into the roles of all involved in delivering the e-Health program, and should cover:
· Stakeholder modelling: identifying and mapping the relationships between all key stakeholders in the program (patients, healthcare professionals, suppliers, delivery partners elsewhere in the public, private and voluntary sector, politicians, the media, etc.); maintaining and updating the stakeholder model on a regular basis;
· A collaborative stakeholder governance model: establishing a clear set of structures, processes and incentives through which the [B2] Program Leadership and the different stakeholders will interact, and covering:
‒ stakeholder participation: ensuring that all stakeholders have a clear understanding of the e-Health program and how they will benefit from it, and have effective and inclusive routes (including through use of digital media) to engage with and participate in the program;
‒ cross-sectoral partnership: engaging effectively with stakeholders from the private, public and voluntary sectors to deliver the program in a way that benefits all sectors;
‒ engagement with other e-Health programs to learn lessons and exchange experience.
v v v
Linkages
Stakeholder Collaboration should be established as a formal workstream within the [B10] Roadmap for Transformation, with measurable performance metrics built into the Benefits Realization framework. Stakeholder engagement underpins all other parts of the e-Health program, because anyone in involved in the realization of the [B1] Vision for Transformation (or receiving benefits as a result) is considered a stakeholder. However, intensive multi-stakeholder engagement is particularly important for [B1] Vision for Transformation, [B2] Program Leadership, [B7] Supplier Partnership, [S2] Brand-led Service Delivery, [S1] Stakeholder Empowerment and [S3] Identity and Privacy Management. The development of successful customer franchises within the [B4] Franchise Marketplace will depend on the effectiveness of collaborative governance – while at the same time helping improve stakeholder collaboration significantly.
5.4 Core Pattern B9 - Common Terminology and Reference Model
Context
In any e-Health programme it is vital that all stakeholders have a common understanding of the key concepts involved and how they interrelate, and have a common language to describe these in.
v v v
The Problem
Leadership and communication both break down when stakeholders understand and use terms and concepts in very different ways, leading to ambiguity, misunderstanding and, potentially, loss of stakeholder engagement.
In everyday life, we use terms – ‘citizen’, ‘need’, ‘service’ – as common, often implicitly accepted labels for concepts. The concept is the abstract mental idea (which should be universal and language independent) to which the term gives a material expression in a specific language. Particularly in an international environment such as global standardization initiatives, the distinction is important as it is common concepts that we wish to work with, not common terms[1].
This distinction also helps avoid common modeling pitfalls. Terms that may seem similar or the same across two or more languages may actually refer to different concepts; or a single term in one language could be understood to refer to more than one concept which another language expresses with discrete terms: For example, the English term ‘service’ can refer to different concepts - an organizational unit (such as ‘Passport Service’ or ‘Emergency Services’) or something that is performed by one for another (such as ‘a dry cleaning service’ or ‘authentication service’), whereas discrete terms are used for the discrete concepts in German (‘Dienst’ or ‘Dienstleistung’ respectively for the two examples above). As the TGF is intended for use anywhere in the world, it is important to ensure that (ideally) global concepts can be transposed and translated and thus understood in other languages: we therefore need to associate an explicit definition with each concept as we do in a dictionary. The TGF uses a standard structure and methodology to create its terminology[2] and we recommend that such an approach should be maintained in any extension of the terminology.
Concepts do not exist in isolation. In addition to clear definitions and agreed terms, It is the broader understanding of the relationships between concepts that give them fuller meaning and allow us to model our world, our business activities, our stakeholders, etc. in a way that increases the chance that our digital systems are an accurate reflection of our work. Any conformant community should be able to use a common terminology without ambiguity and be sure that these terms are used consistently throughout all work.
v v v
The Solution
Ensure that all stakeholders have a clear, consistent and common understanding of the key concepts relating to healthcare in the home and community; how these concepts relate to each other; how they can be formally modeled; and how such models can be leveraged and integrated into new and existing information architectures. It is particularly important that there is a common understanding of the various terms associated with e-devices and their usage. To this end:
Seek agreement among stakeholders to establish and maintain an agreed and shared Common Terminology and Reference Model.
v v v
Linkages
Introduction to Terminology
A core terminology is proposed below and any e-Health program should consider this as a basis for its own terminology and reference model. It should be noted that this glossary is an extension of the main TGF Core Terminology as set out in the Transformational Government Framework (TGF) Version 2.0 and those terms should also be used wherever appropriate.
The TGF does not include a formal ontology but is sufficiently clear in its concepts, definitions and relationships between concepts that subsequent ontology development is possible if so desired.
Each entry below consists of a preferred Term followed by the Definition (indented). Words in bold within a definition refer to other terms defined within this core terminology. Occasionally, a definition is followed by a note to clarify some element of the definition or term.
e-Device
any piece of equipment that is used for environmental control and patient condition monitoring and to and from which patient data is transmitted electronically to healthcare practitioner(s)
e-Health
healthcare practices supported by electronic processes and communication between practitioners and patients using the Internet or other ICT networks
Healthcare
the diagnosis, treatment, and prevention of disease, illness, injury, and other physical and mental impairments in humans
Note: Healthcare is delivered by practitioners in medicine, optometry, dentistry, nursing, pharmacy, allied health, and other care providers. It refers to the work done in providing primary care, secondary care and home and community care, as well as in public health.
Home and community care
the many types of healthcare interventions delivered outside of the primary and secondary care facilities
Note: It includes the services of professionals in residential and community settings in support of self care, home care, long-term care, assisted living, and treatment for substance use disorders and other types of health and social care services.
Internet of Things (IoT)
a world where physical objects are seamlessly integrated into the information network, and where the physical objects can become active participants in business processes.
Note: Services are available to interact with these 'smart objects' over the Internet, query and change their state and any information associated with them, taking into account security and privacy issues.
Primary care
the work of healthcare professionals who act as a first point of consultation for all patients within a healthcare system
Secondary care
the healthcare services provided by medical specialists and other health professionals who generally do not have first contact with patients
5.5 Core Pattern T2 - Technology Development and Management
Context
In order for [T1] Digital Asset Mapping and Management to be effective in aligning healthcare technology and digital assets with the integrated, non-silo based approach set out in [B3] Transformational Operating Model, it is essential to have a top-level vision and architecture for future technology use across the healthcare community.
v v v
The Problem
Technological change is more rapid than organizational change and yet healthcare communities often find themselves locked-in to particular technology solutions. Communities need to protect themselves against the downside of technology evolution by developing a strategic approach to IT that guarantees future agility as markets develop and healthcare priorities change.
Transformational healthcare needs a strategic IT platform to guarantee future agility as patient and practitioner priorities change. Such a platform cannot afford to be locked-in to specific technologies or solutions that prevent or limit such agility.
This means that an e-Health program should establish a blueprint for open, community-wide, service-oriented, interoperable IT. Key features of such a blueprint include:
· a commitment to the paradigm and principles of Service Oriented Architecture (SOA) and SOA-based infrastructure, as defined in the OASIS ‘Reference Model for Service-Oriented Architecture [SOA-RM]. Service-Oriented Architecture must be understood in its broadest sense – as a paradigm for organising and using capabilities distributed and managed across different ownership domains. In this sense, SOA is technology and platform agnostic and thus provides an appropriate foundation for the technology management framework.
· modular design, including the realization of discrete care and services that can perform work on behalf of other parties, underpinned by clear service descriptions and contracts for any capability that is offered for reuse by another party;
· clear ownership and governance for all blueprint elements;
· shared services: managing key ICT building blocks as community-wide resources available as re-usable, shared services - in particular common patient data sets (e.g. name, address); applications and application interfaces (e.g. authentication, payments, notifications); and core ICT infrastructure.
· use of the Internet of Things to connect to and use e-Devices including standards and common approaches for management of the connections and security in line with patient choice and privacy
· published standards to enable safe exchange of information between modules (all open, exportable, and based wherever possible on international standards) and which cover: services; data outcomes; rules; KPIs; interoperability.
· a commitment to enable both privacy and openness: all personal data held securely, and under the ownership and control of the individual patient; all non-personally identifiable public data open for reuse and innovation by third parties;
· tools and resources: standards, metadata, tools, incentives and business models to facilitate transition towards the blueprint architecture by stakeholder organizations.
Such a blueprint is not something that would typically be implemented in a “big bang” or by a single IT supplier, but should:
· provide an agreed architecture on which healthcare organizations and their suppliers can converge over time;
· establish a multi-level competitive landscape at the platform, services and application layers.
v v v
The Solution
TGF programs should therefore work with stakeholders (including government agencies, IT suppliers, SMEs and other delivery partners) to establish and maintain an open, service-oriented, government-wide IT architecture, and to develop a phased migration plan towards that architecture, which:
- concentrates technology resources and efforts around leveraging open standards and SOA Principles so as to ensure development and deployment agility, and support all customer interactions, from face-to-face interactions by frontline staff to online self-service interactions.
- uses the Reference Model for Service-Oriented Architecture [SOA-RM] as the primary source for core concepts and definitions of the SOA paradigm realizes discrete services that can perform work on behalf of other parties, with clear service descriptions and contracts for any capability that is offered for use by another party.
- manages key ICT building blocks as government-wide resources and make them available as re-usable, shared services - in particular common customer data sets (e.g. name, address); applications and application interfaces (e.g. authentication, payments, notifications); and core ICT infrastructure.
· wherever possible prefers interoperable, open standards, particularly when these are well supported in the market-place. Standards of particular relevance in this context are:
- pays due attention to the total cost of ownership and operation of technology and consider the possible value of open source when making technology choices.
v v v
Linkages
Shifting from the current set of legacy IT systems and contractual arrangements to a more integrated, SOA-based approach that supports e-Health in the Home and Community domain will be a multi-year process of change. That process should be built in as a core element of the [B10] Roadmap for Transformation and, in particular, to work on [B7] Supplier Partnership (which is essential in order to ensure that new procurements establish requirements and supplier relationships that help build towards the future vision). And the process will need proactive governance, as described in [T1] Digital Asset Mapping and Management.
The European Interoperability Framework[EIF] has a useful definition of “open” in 5.1.1 “Specifications, openness and reuse”.
The TGF Core Pattern [B6] sets out the requirement to use the Policy Product Matrix to identify all the standards, policies, guidelines etc which are needed to make sure all aspects of a cross-organization interoperability problem (political, legal, organizational, semantic, technical,) are managed effectively. It also advises that the Programme Leadership should undertake a policy gap analysis through Engagement with Stakeholders, and then ensure that the accountability and process for developing any missing Policy Products is embedded within the Roadmap for Transformation.
Most of the TGF Policy Product Types are relevant to the e-Health community. Some are very generic to all domains of public sector activity and require no further explanation in this Profile. The full text of them is available in the Matrix at https://wiki.oasis-open.org/tgf/Policy%20Products
However some are considered essential for e-Health programmes and these are shown in full below suitably tailored for that community.
6.1 Business Management Layer
6.1.1 “Business Management/Political”
|
Policy Product Type - BENEFITS REALIZATION STRATEGY |
|
|
|
Description: The strategy for ensuring that the intended benefits from the e-Health programme are delivered in practice. |
||
|
Problem Addressed: Benefits Realization |
||
|
Example(s)
of current Policy Product of this type: |
||
|
Notes: See TGF v2.0 Section 7 Benefits Realization |
|
Policy Product Type - TRANSFORMATIONAL OPERATING MODEL |
|
|
Description: The strategy for ensuring that the intended benefits from the e-Health programme are delivered in practice. |
|
|
Problem Addressed: Target Business Operating Model |
|
|
Example(s)
of current Policy Product of this type: |
|
|
Notes: See TGF Pattern [B3] Transformational Operating Model as amended in this Profile. |
|
6.1.2 “Business Management/Legal”
|
Policy Product Type - LEGAL AUTHORITY FOR INTER-AGENCY COLLABORATION |
|
|
Description: This represents the legal basis for inter healthcare agency collaboration, data and information exchanges and other joint activities. |
|
|
Problem Addressed: An early step in the Transformation Roadmap for many governments is the identification and redressing of legal barriers. Very often existing laws and practices prohibit full inter-agency working, for example by limiting the ability of an agency to act for tightly prescribed purposes. |
|
|
Example(s) of current Policy Product of this type: None available |
|
|
Notes: National legislation will vary
on this aspect so it will be necessary to consult with Government lawyers to
identify and remove any barriers. |
6.1.3 “Business Management/Organisational”
|
Policy Product Type - BENEFITS REALIZATION PLAN |
|
|
Description: The plan for delivering the Benefits Realization Strategy for the e-Health programme. |
|
|
Problem Addressed: Benefits Realization |
|
|
Example(s) of current Policy Product of this type: |
|
|
Notes: See TGF v2.0 Section 7
Benefits Realization |
|
|
Policy Product Type - COLLABORATIVE STAKEHOLDER ENGAGEMENT MODEL |
|
|
Description: A model that articulates all of these elements: a map all stakeholders, coupled with the structures, engagement processes and incentives needed to deliver full understanding and buy-in to the e-Health programme, plus effective stakeholder action in support of it. |
|
|
Problem Addressed: Stakeholder Engagement |
|
|
Example(s)
of current Policy Product of this type: |
|
|
Notes:
See TGF Pattern [B5] Stakeholder Collaboration as amended in this Profile. |
|
|
Policy Product Type - COMMON TERMINOLOGY AND REFERENCE MODEL |
|
|
Description: The means by which all stakeholders have a common understanding of the key concepts involved in the e-Health programme and how they interrelate, and the common language to describe them. |
|
|
Problem Addressed: Common Language |
|
|
Example(s) of current Policy Product of this
type: |
|
|
Notes: See TGF Pattern [B9] Common Terminology and Reference Model and the e-Health Glossary in this Profile. |
|
|
Policy Product Type - SUPPLIER MANAGEMENT GUIDELINES |
|
|
Description: An e-Health programme requires effective, partnership-based relationships with suppliers, particularly suppliers of e-Devices. Supplier Management guidelines set out a formalized and robust way of managing, monitoring and developing supplier performance. They focus on the overall relationship with the supplier rather than the specific relationship around an individual contract. |
|
|
Problem Addressed: Supplier Management |
|
|
Example(s) of current Policy Product of this type: |
|
|
Notes: See TGF Pattern [B7] Supplier Partnership |
6.1.4 “Business Management/Semantic”
|
Policy Product Type - BUSINESS PROCESS MODEL |
|
|
Description: A model that depicts the business processes of an organization or community. The model typically shows a collection of related, structured activities or tasks that produce a specific service or product for a particular patient or set of patients. It often can be visualized with a flowchart as a sequence of activities. |
|
|
Problem Addressed: Business Processes |
|
|
Example(s)
of current Policy Product of this type: |
|
|
Notes:
See TGF Pattern [T1] Digital Asset and Mapping Management |
|
6.2 Service Management Layer
6.2.1 “Service Management/Political”
|
Policy Product Type - ACCESSIBILITY POLICY |
|
|
Description: The Policy setting out how to make services available to all patients, particularly those with disabilities, including visual, auditory, physical, speech, cognitive, and neurological disabilities. |
|
|
Problem Addressed: Accessibility |
|
|
Example(s) of current Policy Product of this type:
|
|
|
Notes: See TGF Pattern [S4] Channel Management Framework |
|
Policy Product Type - DIGITAL INCLUSION STRATEGY |
|
|
Description: The strategy for ensuring that all patients can enjoy the benefits of the e-Health services through digital channels. Typically, developed in partnership with the private and voluntary sectors, such a strategy will set out the healthcare community’s approach to addressing the key access, confidence and motivation barriers to digital engagement. |
|
|
Problem Addressed: Digital inclusion |
|
|
Example(s) of current Policy Product of this type:
|
|
|
Notes: See TGF Pattern [S4] Channel Management Framework |
|
Policy Product Type - INTERMEDIARIES STRATEGY |
|
|
Description: The strategy for the involvement of private and voluntary sector intermediaries in the delivery of e-Health services. |
|
|
Problem Addressed: Use of Intermediaries |
|
|
Example(s) of current Policy Product of this type:
|
|
|
Notes: See TGF Pattern [S4] Channel Management Framework |
|
|
Policy Product Type - PRIVACY AND DATA SHARING POLICY |
|
|
Description: The government or healthcare community policy for the sharing of data between practitioners, whilst at the same time respecting the needs for data privacy of patients’ records. |
|
|
Problem Addressed: Data Privacy and Sharing |
|
|
Example(s) of current Policy Product of this type: |
|
|
Notes: See TGF Pattern [S3] Identity and Privacy Management |
|
6.2.2 “Service Management/Semantic”
|
Policy Product Type - ACCCESSIBILITY GUIDELINES |
|
|
Description: Guidelines setting out how to make content available to all patients, particularly those with disabilities, including visual, auditory, physical, speech, cognitive, and neurological disabilities. |
|
|
Problem Addressed: Accessibility |
|
|
Example(s) of current Policy Product of this type:
|
|
|
Notes: See TGF Pattern [S4] Channel Management Framework |
|
Policy Product Type - COMMON DATA STANDARDS |
|
|
Description: A set of the most common data items in use by the healthcare community. For each item there should be a full definition together with any appropriate formatting and coding. |
|
|
Problem Addressed: Data Management |
|
|
Example(s)
of current Policy Product of this type: |
|
|
Notes: See TGF Pattern [T2] Technology Development and Management as amended in this Profile. |
|
6.2.3 “Service Management/Technical”
|
Policy Product Type - ACCESSIBILITY STANDARDS |
|
Description: A set of guidelines setting out the standards to be used to ensure maximum inclusivity of e-Health services. |
|
Problem Addressed: Accessibility |
|
Example(s) of current Policy Product of this type:
|
|
Notes: See TGF Pattern [T2] Technology Development and Management |
|
Policy Product Type - SERVICE DEFINITION FOR ONE STOP SERVICES |
|
|
Description: e-Health programmes typically involve a shift from silo-based delivery towards an integrated, multi-channel, patient centric service delivery platform offering “one stop” service delivery and self-help for healthcare. Developing such a service requires a clear end-to-end service definition: a comprehensive documentation describing the product which will be offered to all patients. |
|
|
Problem Addressed: One stop service delivery |
|
|
Example(s) of current Policy Product of this type: None available |
|
|
Notes: See TGF Pattern [B3] Transformational Operating Model as amended in this Profile. |
|
Policy Product Type - SINGLE SIGN-ON ARCHITECTURE |
|
|
Description: The architecture that sets out how patients can access all the services and self help facilities they require through a single sign-on facility. |
|
|
Problem Addressed: Single sign-on |
|
|
Example(s) of current Policy Product of this type: None available |
|
|
Notes: See TGF Pattern [T2] Technology Development and Management as amended in this Profile. |
|
6.3 Technical and Digital Asset Management Layer
6.3.1 “Technical and Digital Asset Management/Political”
|
Policy Product Type - INFORMATION SECURITY STRATEGY |
|
|
Description: The policy for the security of the healthcare communities’ information assets. This should cover not only the hard copies of documents and other paper materials but also web pages and online services and the information captured by them. |
|
|
Problem Addressed: Information Security |
|
|
Example(s) of current Policy Product of this type:
|
|
|
Notes: See TGF Pattern [T1] Digital Assets Mapping and Management as amended in this profile. |
|
6.3.2 “Technical and Digital Asset Management/Organizational”
|
Policy Product Type - OPEN STANDARDS PROCEDURES |
|
|
Description: A set of procedures that allow (the need for) open standards to be raised and lead into a process for filtering requests, defining the need, selecting or building them, adopting them and managing them through to retirement. |
|
|
Problem Addressed: Use of open standards |
|
|
Example(s) of current Policy Product of this type:
Australian Government National Standards Framework - http://www.finance.gov.au/publications/national-standards-framework/index.html |
|
|
Notes: See TGF Pattern [T2] Technology Development and Management as amended in this Profile. |
|
6.3.3 “Technical and Digital Asset Management/Technical”
|
Policy Product Type - APPLICATIONS ARCHITECTURE |
|
|
Description: An architecture that sets out how a suite of applications are being used by the e-Health programme to create a composite application that is scalable, reliable, available and manageable. It is specified on the basis of business and functional requirements. |
|
|
Problem Addressed: IT Management |
|
|
Example(s) of current Policy Product of this type:
|
|
|
Notes: See TGF Pattern [T2] Technology Development and Management as amended in this Profile. |
|
Policy Product Type - NETWORK ARCHITECTURE |
|
|
Description: An architecture showing the design of the communications network for the e-Health programme. Usually the Internet would be used as the network but if an alternative is used then there is the need for the specification of the network's physical components and their functional organization and configuration, its operational principles and procedures, as well as data formats used in its operation. |
|
|
Problem Addressed: Network Management |
|
|
Example(s) of current Policy Product of this type:
|
|
|
Notes: See TGF Pattern [T2] Technology Development and Management as amended in this Profile. |
|
|
Policy Product Type - SECURITY ARCHITECTURE |
|
|
Description: An architecture supporting the development of security for e-Health services by providing illustrations and guidance on how a security framework and related documents would be applied for particular illustrative on-line business scenarios at various levels of trust with currently available technologies and processes. |
|
|
Problem Addressed: Security Management |
|
|
Example(s) of current Policy Product of this type:
|
|
|
Notes: See TGF Pattern [T2] Technology Development and Management as amended in this Profile. |
The following individuals have participated in the creation of this specification and are gratefully acknowledged:
Participants:
Hans A Kielland Aanesen, Individual Member
Oliver Bell, Microsoft Corporation
John Borras, Individual Member
Peter F Brown, Individual Member
Nig Greenaway, Fujitsu Ltd
Jenny Huang, ifOSS Foundation
Gershon Janssen, Individual Member
Chris Parker, CS Transform Ltd
Colin Wallis, New Zealand Government
Joe Wheeler, MTG Management Consultants, LLC
Mark Woodward, Individual Member
In addition we acknowledge the contributions from the OASIS BCM and CAM Technical Committees.
|
Revision |
Date |
Editor(s) |
Changes Made |
|
01 |
7th June 2013 |
John Borras Hans A. Kielland Aanesen |
Initial draft |
|
02 |
23rd January 2014 |
John Borras Hans A. Kielland Aanesen |
Revisions to bring the CN into line with the new TGF v2.0 |
|
03 |
15th March 2014 |
Nig Greenaway |
Revised to reference the Internet of Things and to strengthen patient choice and privacy considerations. |
|
04 |
22 April 2014 |
John Borras Nig Greenaway |
Changes to Figs 3 and 4 to reflect Healthcare services. |